
The impact of geographical access challenges on outcomes of postmastectomy breast reconstruction
Introduction
Breast reconstruction (BR) has been shown to improve psychosocial well-being in women who undergo mastectomy for breast cancer (1-4). The Women’s Health and Cancer Rights Act of 1998 helped to establish insurance coverage for all postmastectomy BR services, including symmetrizing surgery on the contralateral breast and revision procedures required to achieve good aesthetic results (5). Despite this, only 45% of women treated with mastectomy undergo BR, according to a recent analysis of a national database (6). Furthermore, several studies have shown that disparities in the rates of BR among patients who have undergone mastectomy align with specific socioeconomic and demographic factors. Older age (6-9), African American and Latino race (6,9-17), and public insurance (9,11,13,16) have each been independently correlated with reduced rates of BR. Geographical access to a plastic surgeon is another predictor of postmastectomy BR, with patients from rural areas significantly less likely to have reconstruction compared to their urban counterparts (13,18-23). The asymmetric distribution of plastic surgeons across the United States, with clusters in urban and academic environments, creates an access challenge for individuals living in rural areas who might benefit from reconstructive surgical care (24).
While the relationship between geographical access and whether or not a woman will undergo BR has been well-studied, comparatively little is known about how travel distance affects the quality of reconstruction or complication rates. Our institution, a small academic medical center in northern New England, routinely performs postmastectomy BR for patients who live throughout a large geographical area spanning Vermont and much of upstate New York. We hypothesized that, compared to patients who live within our hospital’s metropolitan area, patients traveling from further away for BR would be at risk for delayed diagnosis of post-operative complications, less frequent follow-up, and aesthetically poorer long-term results. In this study, we sought to determine whether greater travel distance from home to the plastic surgery center was associated with poorer BR outcomes. We present the following article in accordance with the STROBE reporting checklist (available at https://abs.amegroups.com/article/view/10.21037/abs-22-32/rc).
Methods
Study design
We conducted a retrospective review of all patients who underwent postmastectomy BR at the University of Vermont Medical Center (UVMMC) from 2015 to 2019. A total of 345 patients were identified via Current Procedural Terminology (CPT) codes associated with alloplastic (i.e., implant-based) or autologous (i.e., using an individual’s own tissue) forms of BR surgery. Patients were excluded if they had not received an index (i.e., not revisionary) BR surgery during the study period following a prior mastectomy performed for cancer or risk of cancer. Of these patients, 291 had been followed for at least 180 days post-BR and were included in the analysis. Data elements related to patient demographics, health characteristics, cancer type and treatment, BR technique, and post-operative follow-up were collected.
Patients were divided into two cohorts (Far and Not Far) based on the location of their home zip code as recorded in the electronic medical record. For all subjects, travel time was calculated by measuring the time required to drive from the center of their home zip code to UVMMC according to Google Maps (Google, Mountain View, CA, USA). The two cohorts were split at the median travel time across all subjects; Not Far patients lived within 41 minutes of our institution; Far patients lived more than 41 minutes away. All plastic surgery facilities at our institution are located within a two-mile radius of the main hospital. All driving time estimates were retrieved without accounting for traffic, which is not a major obstacle in our region. Driving time was used instead of driving distance or Euclidian distance because it more accurately represents the challenges our patients navigate to reach our hospital; routes often include ferries and/or small, low-speed roads.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Institutional Review Board of The University of Vermont and UVMMC (No. IRB00000485) and individual consent for this retrospective analysis was waived.
Patient characteristics
Baseline characteristics and demographic variables retrieved from the electronic chart consisted of age, body mass index (BMI), medical comorbidities, smoking status, race, insurance type, and home zip code. Factors related to breast cancer and cancer treatment were recorded: American Joint Committee on Cancer (AJCC) stage, BRCA gene status, chemotherapy and radiation therapy schedule, and mastectomy type. Relevant data pertaining to the BR was also collected: timing (immediate vs. delayed), laterality, and reconstruction type (alloplastic vs. autologous). Autologous BR was further subdivided into free flap (muscle sparing transverse rectus abdominis myocutaneous flap or deep inferior epigastric artery perforator flap), other autologous (latissimus dorsi or other local flap), or combination autologous/alloplastic (local or free flap plus tissue expander or implant for additional volume) reconstruction categories.
Study outcomes
This study aimed to measure associations between patient geography and BR outcomes. These outcomes included post-operative complications, follow-up timing and frequency, and number of revision procedures. The post-operative complications we queried for were seroma, infection, hematoma, fat necrosis, and breast skin necrosis. Hospital readmissions due to a complication of BR were also noted. A follow-up was defined as a post-operative visit at the plastic surgery clinic (located in close proximity to the surgical center) for any reason, excluding appointments solely scheduled for tissue expander filling.
Revision procedures encompassed surgical or non-surgical interventions performed by a plastic surgeon for the purpose of improving the aesthetic outcome of BR. These procedures were: nipple-areola complex (NAC) reconstruction, nipple and areola tattooing, fat grafting, peri-incisional skin revision, scar revision, triamcinolone injection, and symmetrizing operations performed on the contralateral breast after an initial unilateral BR. For analyses in which the outcome variable was related to revision procedures, nipple-sparing mastectomy patients were excluded, as NAC reconstruction and tattooing comprised a significant fraction of all revision procedures. Additionally, patients with less than 1.5 years of follow-up were excluded from revision procedures analyses as the BR process is commonly considered complete at two years after the primary operation (25).
Statistical analysis and maps
The Far and Not Far cohorts were first compared via univariate analysis across a number of patient characteristics and outcomes variables using a linear analysis of variance (ANOVA) model for continuous variables and Pearson’s chi-squared test for categorical variables. Multivariate analysis was then performed to quantify the independent impact of patient geography (whether a patient belonged to the Far or Not Far cohort) on BR outcomes, relative to other potentially explanatory variables. Effects on categorical outcomes (e.g., any complication-related hospital readmission) were expressed as odds ratios (ORs) and 95% confidence intervals (CIs) calculated using a logistic regression model. Effects on continuous variable outcomes (e.g., first follow-up delay, number of follow-ups, number of revision procedures) were expressed as coefficients and 95% CI of a linear regression model. Statistical significance was set at P<0.05. All statistical analyses were performed using R Statistical Software (Foundation for Statistical Computing, Vienna, Austria).
Maps were generated using ArcGIS Pro 2.6.1 (Environmental Systems Research Institute, Redlands, CA) on the WGS84 Web Mercator (Auxiliary Sphere) coordinate system and 1:2,500,000 scale. Datasets were added using ArcGIS World Geocoding Service with individual zip codes as inputs. In very rare instances of irretrievable data, missing elements were omitted from the analysis altogether. Each dataset was then categorized into relevant classes using the “Quantile” method. Data points with identical zip codes were dispersed using “Disperse Marker” tool with expanded dispersal pattern, 0.25 point minimum spacing, and 1:2,000,000 reference scale as parameters.
Results
A total of 291 women underwent postmastectomy BR at UVMMC from 2015 to 2019 (Figure 1). The median travel time was 41 minutes; 146 patients lived within a 41-minute drive of the medical center (Not Far), 145 patients lived further from our institution (Far) (Figure 1). Eighty-five patients lived within 20 minutes of UVMMC, four patients traveled from more than 230 minutes away (Figures 1,2). The Not Far and Far groups were statistically similar in terms of average age, BMI, diabetes, and smoking status (Table 1). More Stage I cancer was diagnosed compared to Stage 0 cancer in Not Far patients and vice versa in Far patients (P=0.016). Otherwise, there were no significant differences between the groups in terms of breast cancer treatment, mastectomy type, timing of reconstruction following mastectomy, BR type (free flap vs. other autologous vs. alloplastic), or length of stay. Of the patients studied, 97.3% were of white race, consistent with Vermont’s 94.2% white population as of 2019 (26). There were no differences in terms of insurance providers between the groups. There was no significant difference in the overall length of follow-up between the Far and Not Far groups. The minimum length of follow-up among all subjects was 181 days with an average period of over two years.
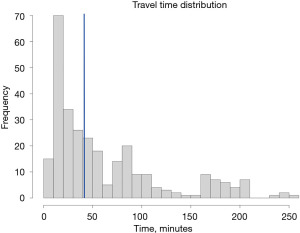
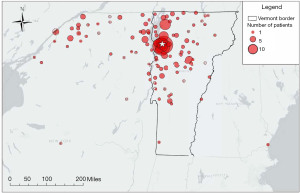
Table 1
| Characteristics | Not Far (N=146) | Far (N=145) | Total (N=291) | P |
|---|---|---|---|---|
| Age (years) | 0.898 | |||
| Mean (SD) | 49.9 (10.5) | 50.1 (11.5) | 50.0 (11.0) | |
| BMI (kg/m2) | 0.034 | |||
| Mean (SD) | 27.3 (6.0) | 28.8 (6.0) | 28.0 (6.0) | |
| Diabetes | 0.098 | |||
| Yes | 4 (2.7%) | 10 (6.9%) | 14 (4.8%) | |
| No | 142 (97.3%) | 135 (93.1%) | 277 (95.2%) | |
| Smoking status | 0.924 | |||
| Former | 58 (39.7%) | 58 (40.3%) | 116 (40.0%) | |
| Never | 88 (60.3%) | 86 (59.7%) | 174 (60.0%) | |
| AJCC stage | 0.016 | |||
| 0 | 27 (21.8%) | 43 (38.1%) | 70 (29.5%) | |
| I | 58 (46.8%) | 33 (29.2%) | 91 (38.4%) | |
| II | 32 (25.8%) | 32 (28.3%) | 64 (27.0%) | |
| III | 7 (5.6%) | 5 (4.4%) | 12 (5.1%) | |
| BRCA | 0.273 | |||
| No | 120 (82.2%) | 106 (74.6%) | 226 (78.5%) | |
| BRCA1 | 6 (4.1%) | 10 (7.0%) | 16 (5.6%) | |
| BRCA2 | 20 (13.7%) | 26 (18.3%) | 46 (16.0%) | |
| Chemotherapy | 0.289 | |||
| None | 63 (43.2%) | 75 (52.1%) | 138 (47.6%) | |
| Before reconstruction | 47 (32.2%) | 39 (27.1%) | 86 (29.7%) | |
| During or after reconstruction | 20 (13.7%) | 21 (14.6%) | 41 (14.1%) | |
| Both | 16 (11.0%) | 9 (6.3%) | 25 (8.6%) | |
| Radiation therapy | 0.367 | |||
| Before reconstruction | 32 (21.9%) | 35 (24.1%) | 67 (23.1%) | |
| During or after reconstruction | 24 (16.4%) | 23 (15.9%) | 47 (16.2%) | |
| Both | 9 (6.2%) | 3 (2.1%) | 12 (4.1%) | |
| Mastectomy type | 0.213 | |||
| Partial | 11 (7.5%) | 19 (13.2%) | 30 (10.4%) | |
| Nipple sparing | 16 (11.0%) | 10 (6.9%) | 26 (9.0%) | |
| Skin sparing | 39 (26.9%) | 45 (31.3%) | 84 (29.1%) | |
| Simple or radical | 79 (54.5%) | 70 (48.6%) | 149 (51.6%) | |
| Timing of reconstruction | 0.593 | |||
| Immediate | 112 (76.7%) | 115 (79.3%) | 227 (78.0%) | |
| Delayed | 34 (23.3%) | 30 (20.7%) | 64 (22.0%) | |
| Reconstruction type | 0.475 | |||
| Free flap | 23 (15.8%) | 33 (22.8%) | 56 (19.2%) | |
| Other autologous | 8 (5.5%) | 9 (6.2%) | 17 (5.8%) | |
| Combination autologous/alloplastic | 8 (5.5%) | 7 (4.8%) | 15 (5.2%) | |
| Alloplastic | 107 (73.3%) | 96 (66.2%) | 203 (69.8%) | |
| Race | 0.343 | |||
| White | 141 (96.6%) | 142 (97.9%) | 283 (97.3%) | |
| Asian | 3 (2.1%) | 0 (0.0%) | 3 (1.0%) | |
| Hispanic | 1 (0.7%) | 2 (1.4%) | 3 (1.0%) | |
| Other | 1 (0.7%) | 1 (0.7%) | 2 (0.7%) | |
| Insurance type | 0.407 | |||
| Private | 108 (74.0%) | 110 (75.9%) | 218 (74.9%) | |
| Medicaid | 9 (6.2%) | 11 (7.6%) | 20 (6.9%) | |
| Medicare | 24 (16.4%) | 23 (15.9%) | 47 (16.2%) | |
| Tricare | 5 (3.4%) | 1 (0.7%) | 6 (2.1%) | |
| Length of stay (days) | 0.129 | |||
| Mean (SD) | 1.9 (1.7) | 2.3 (2.1) | 2.1 (1.9) | |
| Length of follow up (days) | 0.871 | |||
| Mean | 818 | 827 | 823 | |
| Range | 367–1,826 | 181–1,790 | 181–1,826 |
BMI, body mass index; AJCC, American Joint Committee on Cancer.
Greater travel time was associated with less prompt and less frequent follow-up (Table 2). There was a greater delay in being seen at the plastic surgery clinic following hospital discharge among patients who traveled from further away (5.9±2.4 vs. 7.0±3.0, P=0.001; mean ± SD, Not Far vs. Far). On average, more days had elapsed between the diagnosis of a BR complication and the previous follow-up visit in patients who lived further away (6.8±9.0 vs. 24.6±59.2, P=0.014). Greater travel time was also associated with fewer follow-up visits at six months post-op (9.8±4.4 vs. 8.5±3.6, P=0.012) and at one year (13.7±5.9 vs. 11.8±5.3, P=0.004). On multivariate linear regression analysis, being a Far patient accounted for 2.13 (P=0.007) or 2.44 (P=0.070) fewer follow-up visits within one year of alloplastic (R2=26%) or autologous (R2=38%) BR, respectively (Tables 3,4). Only hospital readmission was consistently associated with a greater number of follow-ups; having private insurance did not have a significant effect.
Table 2
| Variables | Not Far (N=146), mean (SD) | Far (N=145), mean (SD) | P value |
|---|---|---|---|
| Days between discharge and first follow-up | 5.9 (2.4) | 7.0 (3.0) | 0.001 |
| Days between diagnosis of first complication and previous follow-up | 6.8 (9.0) | 24.6 (59.2) | 0.014 |
| Days between diagnosis of first complication and most recent hospital discharge | 31.1 (89.5) | 50.4 (89.0) | 0.222 |
| Outpatient follow-up visits within 6 months of surgery | 9.8 (4.4) | 8.5 (3.6) | 0.012 |
| Outpatient follow-up visits within 1 year of surgery | 13.7 (5.9) | 11.8 (5.3) | 0.004 |
Table 3
| Variables | Outpatient follow-ups in 1 year (alloplastic) | ||
|---|---|---|---|
| Coefficient | 95% CI | P | |
| Far vs. Not Far | −2.13 | −3.67 to −0.60 | 0.007 |
| Age | 0.00 | −0.07 to 0.07 | 0.974 |
| Length of stay | 0.51 | −0.23 to 1.24 | 0.174 |
| Chemotherapy | −0.36 | −2.14 to 1.42 | 0.693 |
| Radiation | −0.27 | −2.13 to 1.60 | 0.776 |
| Hospital readmission | 5.00 | 3.39 to 6.61 | <0.001 |
| Returns for revision procedures | 0.78 | 0.01 to 1.56 | 0.048 |
| Private insurance | 1.77 | 0.08 to 3.47 | 0.041 |
Observations: 178. R2/R2 adjusted: 26.0%/22.5%. CI, confidence interval.
Table 4
| Variables | Outpatient follow-ups in 1 year (autologous) | ||
|---|---|---|---|
| Coefficient | 95% CI | P | |
| Far vs. Not Far | −2.44 | −5.09 to 0.21 | 0.070 |
| Age | 0.07 | −0.06 to 0.20 | 0.313 |
| Length of stay | 0.72 | 0.17 to 1.27 | 0.011 |
| Chemotherapy | 0.20 | −2.92 to 3.31 | 0.901 |
| Radiation | 4.02 | 0.84 to 7.19 | 0.014 |
| Hospital readmission | 5.17 | 2.40 to 7.94 | <0.001 |
| Returns for revision procedures | 0.60 | −0.29 to 1.48 | 0.184 |
| Private insurance | 2.54 | −0.52 to 5.59 | 0.102 |
Observations: 73. R2/R2 adjusted: 37.6%/29.8%. CI, confidence interval.
Among women who had undergone non-nipple-sparing mastectomy with at least 1.5 years of follow-up, Not Far patients received more revision procedures compared to Far patients following both autologous (2.00±1.39 vs. 1.74±1.48, P=0.474) and alloplastic (1.27±1.10 vs. 0.47±0.83, P<0.001) reconstruction (Table 5). On multivariate regression analysis (Table 6; R2=24%), compared to being Not Far, being a Far patient independently accounted for an average of 0.64 fewer revision procedures (P<0.001). Among other tested variables, only having an autologous BR (β=1.05, P<0.001) was associated with a significant difference in the number of revision procedures; having private insurance approached statistical significance (β=0.35, P=0.055).
Table 5
| Reconstruction type | Not Far (N=119) | Far (N=116) | P |
|---|---|---|---|
| Autologous (N=70) | 0.474 | ||
| Mean (SD) | 2.00 (1.39) | 1.74 (1.48) | |
| Alloplastic (N=114) | <0.001 | ||
| Mean (SD) | 1.27 (1.10) | 0.47 (0.83) |
Table 6
| Variables | Returns for revision procedures | ||
|---|---|---|---|
| Coefficient | 95% CI | P | |
| Far vs. Not Far | −0.64 | −0.95 to −0.33 | <0.001 |
| Age | 0.01 | −0.01 to 0.02 | 0.353 |
| BMI | 0.01 | −0.01 to 0.04 | 0.320 |
| Diabetes | −0.36 | −1.03 to 0.31 | 0.287 |
| Radiation | −0.19 | −0.51 to 0.13 | 0.251 |
| Bilaterality | 0.32 | 0.00 to 0.64 | 0.047 |
| Autologous reconstruction | 1.05 | 0.70 to 1.41 | <0.001 |
| Hospital readmission | −0.16 | −0.50 to 0.18 | 0.356 |
| Private insurance | 0.35 | −0.01 to 0.71 | 0.055 |
Observations: 207. R2/R2 adjusted: 24.1%/20.6%. BMI, body mass index; CI, confidence interval.
In general, the rates of BR complications were not significantly different between the Not Far and Far groups (Table 7). Among alloplastic BR patients, Not Far patients were diagnosed with seroma more frequently (26.2% vs. 14.6%, P=0.042). Otherwise, there were no statistically significant differences in complication rates between the cohorts.
Table 7
| Reconstruction type | Complication | Not Far (N=146) | Far (N=145) | P |
|---|---|---|---|---|
| Autologous (N=88) | Length of stay (days), mean (SD) | 3.6 (2.2) | 4.2 (2.5) | 0.216 |
| Seroma | 8 (20.5%) | 10 (20.4%) | 0.990 | |
| Infection | 7 (17.9%) | 11 (22.4%) | 0.603 | |
| Hematoma | 2 (5.1%) | 4 (8.3%) | 0.557 | |
| Fat necrosis | 6 (15.4%) | 4 (8.2%) | 0.289 | |
| Breast skin necrosis | 4 (10.3%) | 11 (22.4%) | 0.131 | |
| Complication-related hospital readmission | 7 (17.9%) | 15 (30.6%) | 0.173 | |
| Alloplastic (N=202) | Length of stay (days), mean (SD) | 1.3 (1.0) | 1.3 (0.9) | 0.700 |
| Seroma | 28 (26.2%) | 14 (14.6%) | 0.042 | |
| Infection | 21 (19.6%) | 14 (14.6%) | 0.342 | |
| Hematoma | 10 (9.3%) | 7 (7.3%) | 0.598 | |
| Fat necrosis | 7 (6.5%) | 4 (4.2%) | 0.455 | |
| Breast skin necrosis | 19 (17.8%) | 19 (19.8%) | 0.711 | |
| Complication-related hospital readmission | 23 (21.5%) | 28 (29.2%) | 0.208 |
Discussion
Despite an abundance of evidence showing that BR is beneficial to women who undergo oncologic mastectomy (1-4), disparities in rates of reconstruction persist along lines of race, insurance status, and geography (6,9-23,27). Studies have shown that patients who live in rural areas, and especially patients who live far from academic hospitals, are significantly less likely to receive BR (20,23,27,28). Our institution, the UVMMC, occupies a unique position among plastic surgery providers, offering complex microsurgical options to a largely rural patient population. As a result, we are able to study plastic surgery-related outcomes in a cohort that is split among the metropolitan area surrounding our medical center, more rural parts of Vermont, and the expansive Adirondack region of upstate New York. While the literature supports the significance of multiple factors in influencing whether or not a patient undergoes postmastectomy BR, comparatively little is known about how those factors affect BR quality and safety. To our knowledge, this is the first study assessing the impact of patient geography on BR outcomes.
Of the 291 patients who underwent BR at our institution from 2016 to 2019, half lived more than 41 minutes away from our surgical center and plastic surgery clinic (Table 1, Figure 1). That Far cohort largely represented a group of patients who traveled from rural Vermont or upstate New York to reach our medical center (Figure 2). While the Not Far group included 85 patients who lived within 20 minutes of our hospital, patients in the Far cohort sometimes traveled from more than three hours away, presenting an obvious challenge to attending post-operative visits. Indeed, our analysis showed that greater travel distance was associated with a longer delay between hospital discharge and the first follow-up appointment; there was also a longer span between the diagnosis of a first complication and the previous outpatient visit in that group (Table 2). Non-infectious complications of both autologous and alloplastic BR most commonly occur at 2 to 15 days following surgery, highlighting the clinical importance of prompt follow-up after hospital discharge (29). Additionally, a lack of appropriately frequent follow-up after BR may result in the progression of minor complications (e.g., cellulitis, epidermolysis) to more serious ones (e.g., implant infection, mastectomy flap necrosis) in the absence of evaluation by a plastic surgeon. Although there were few significant differences in the incidence of complications between the two groups (Table 7), we hypothesize that there were more undiagnosed minor complications in Far patients, who were seen less frequently overall (Table 2). This idea is supported by the finding that significantly more seromas were diagnosed in Not Far alloplastic BR patients vs. Far. Future analysis should evaluate the severity of BR complications in addition to incidence.
Compared to patients in the Not Far cohort, Far patients received approximately 0.8 fewer revision procedures for alloplastic BR performed after non-nipple-sparing mastectomy (Table 5). BR is commonly considered by plastic surgeons to be a multi-stage process, requiring operations subsequent to the primary procedure to achieve a good aesthetic result (30-32). In our analysis, patient geography (being Far vs. being Not Far) and type of reconstruction (autologous vs. alloplastic) had, by far, the most significant effects on the number of revision procedures patients received (Table 6). Otherwise, only bilaterality of the reconstruction was also associated with a (less) significant effect. These associations were isolated among other factors that included age, BMI, diabetes, radiation therapy, hospital readmission, and insurance type. While previous studies have shown that women receive an average of two to three revision procedures following BR (25,31,33), the Far cohort in our study received only 1.74 or 0.47 revisions after autologous or alloplastic reconstruction, respectively (Table 5). There are several potential explanations for the relative lack of revision procedures received by Far patients: more remote patients were seen less frequently in follow-up, and may have, therefore, been offered revision less often; Far patients may also have been less interested in minor aesthetic improvements that would require significant travel. Future studies will attempt to further characterize the specific motivations underlying this observed divergence; regardless, our results show that geographical access was likely a major contributor to the disparity in number of revision procedures received by patients in our two cohorts.
Few studies have sought to identify sources of disparity in relation to BR revision procedures. Odom et al. studied the relationship between NAC reconstruction and payor and found no correlation between number of revisions and insurance type, a result our analysis supports (33). Orr and colleagues, meanwhile, found that Caucasian race was predictive of a greater numbers of revisions (34). Our results add travel distance to the list of factors that may impact the probability of attaining a satisfactory BR result. Evidence that post-BR revisions have significant impact on breast satisfaction and psychosocial well-being underscores the importance of identifying factors that affect the receipt of revision procedures (35-37). While much of the published research on the topic of BR disparities has focused on whether or not patients receive reconstruction at all, this study implies that variables like travel distance continue to affect outcomes even after patients enter the BR pathway.
The plastic surgeons at our institution are well-aware of the geographic and logistical challenges many of our patients face and elicit information about living situation, access to transportation, and reconstructive goals as part of the pre-operative planning process. Our emphasis on providing noninferior care to more remote patients is evidenced by this study’s lack of significant differences in reconstruction timing (immediate vs. delayed) and type (autologous vs. alloplastic) seen in other studies on geographical access challenges (13,19,27,28). Moreover, disparities in follow-up frequency and number of revision procedures may result from a combination of subconscious surgeon biases and intentional patient decisions. We acknowledge that the relationships between distance, follow-up attendance and timing, complication rates, and revision procedures are likely multidirectional and nuanced beyond the detail included in this study. Still, we suggest that, especially when approaching patient populations dispersed across large geographical areas, plastic surgeons emphasize the importance of follow-up especially during periods of high risk for complications (2 to 15 days post-operation) and at any sign of infection. Additionally, surgeons should explain the multi-stage nature of BR and the travel implications for patients who live far away and desire an optimal aesthetic result.
Finally, while other studies have suggested increasing the number of plastic surgeons operating in rural areas (19,20,23), we would further advocate for increased utilization of telemedicine, which has been shown to be an effective method for improving post-operative care following microsurgical procedures among patients who live far from major medical centers (38). As access to high-fidelity video conferencing technology has become more widespread in the wake of the coronavirus 2019 (COVID-19) pandemic, plastic surgeons should increasingly use telemedicine to discuss common complaints following surgery and collaborate with patients on next steps (39). Telemedicine was not utilized by our surgeons during the study period, but has been rapidly implemented since then with positive feedback from patients. Though not an ideal replacement for many in-person clinic visits, telemedicine offers a convenient way for patients to communicate with their surgeons without traveling over long distances (40,41). Future studies will re-examine the impact of geographical access on BR outcomes to determine whether the wide adoption of telemedicine has alleviated any of the disparities found in our pre-COVID-19 analysis.
Our study has some limitations. It was a retrospective review including multiple surgeons and inherent biases are unavoidable. The racial homogeneity of our population is an advantage in terms of isolating geography as an independent variable but limits the direct applicability of our results to some other environments. Additionally, the lack of an insurance-type effect on BR outcomes may be partly attributable to the relatively generous public insurance policies that exist in Vermont. While our patient population faces travel challenges specific to northern New England (such as low-speed roads and frequently inclement weather), the lack of traffic in our region may limit the generalizability of our findings to plastic surgery centers serving patients in similarly rural catchment areas. Though the cohorts in our study were defined by driving time (instead of linear distance) to account for certain geographical obstacles, the collection of additional information could better characterize the travel challenges encountered by some of our patients. Future, prospective studies should collect data on access to transportation and social support as key factors in determining a patient’s ability to travel for plastic surgery care. Although the majority of BR complications occur in the early post-operative period, our six-month follow-up inclusion criterion is insufficient to reliably capture all possible adverse events (eg, capsular contracture, delayed seroma) which can occur many years after surgery. Finally, while many studies, including ours, take partly for granted the notion that groups who receive more revision procedures have better aesthetic results, this is an assumption that should be validated. Future studies will include patient-reported outcomes to evaluate how satisfaction with BR varies according to patient geography and whether satisfaction is associated with the quantity of revision procedures among these patients.
Conclusions
This study builds upon previous research demonstrating that travel distance is an independent predictor for whether or not a patient will undergo postmastectomy BR. Here, we show that patients who overcome geographical challenges to have BR with a plastic surgeon are seen in follow-up less promptly and less frequently after surgery and receive fewer revision procedures compared to more local patients. Plastic surgeons should be aware of these associations and take travel into account when educating patients on expectations for follow-up and revision procedures. Future studies will seek to determine whether the wide adoption of telemedicine after 2019 has helped to alleviate any of the disparities identified here.
Acknowledgments
The authors thank Bayu Ahmad (Department of Chemistry and Biochemistry, Middlebury College, Middlebury, VT) for his help in generating the geospatial mapping figures included in this article.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://abs.amegroups.com/article/view/10.21037/abs-22-32/rc
Data Sharing Statement: Available at https://abs.amegroups.com/article/view/10.21037/abs-22-32/dss
Peer Review File: Available at https://abs.amegroups.com/article/view/10.21037/abs-22-32/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://abs.amegroups.com/article/view/10.21037/abs-22-32/coif). The authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wilkins EG, Cederna PS, Lowery JC, et al. Prospective analysis of psychosocial outcomes in breast reconstruction: one-year postoperative results from the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg 2000;106:1014-25; discussion 1026-7. [Crossref] [PubMed]
- Rowland JH, Desmond KA, Meyerowitz BE, et al. Role of breast reconstructive surgery in physical and emotional outcomes among breast cancer survivors. J Natl Cancer Inst 2000;92:1422-9. [Crossref] [PubMed]
- Rowland JH, Holland JC, Chaglassian T, et al. Psychological response to breast reconstruction. Expectations for and impact on postmastectomy functioning. Psychosomatics 1993;34:241-50. [Crossref] [PubMed]
- Elder EE, Brandberg Y, Björklund T, et al. Quality of life and patient satisfaction in breast cancer patients after immediate breast reconstruction: a prospective study. Breast 2005;14:201-8. [Crossref] [PubMed]
- 105th Congress (1997) Department of Health and Human Services, Centers for Medicare and Medicaid Services. H.R. 616: Women’s Health and Cancer Rights Act (WHCRA). (Congressional Research Service). Available online: https://www.congress.gov/bill/105th-congress/senate-bill/249/text
- Butler PD, Nelson JA, Fischer JP, et al. Racial and age disparities persist in immediate breast reconstruction: an updated analysis of 48,564 patients from the 2005 to 2011 American College of Surgeons National Surgery Quality Improvement Program data sets. Am J Surg 2016;212:96-101. [Crossref] [PubMed]
- August DA, Wilkins E, Rea T. Breast reconstruction in older women. Surgery 1994;115:663-8. [PubMed]
- In H, Jiang W, Lipsitz SR, et al. Variation in the utilization of reconstruction following mastectomy in elderly women. Ann Surg Oncol 2013;20:1872-9. [Crossref] [PubMed]
- Kruper L, Holt A, Xu XX, et al. Disparities in reconstruction rates after mastectomy: patterns of care and factors associated with the use of breast reconstruction in Southern California. Ann Surg Oncol 2011;18:2158-65. [Crossref] [PubMed]
- Tseng WH, Stevenson TR, Canter RJ, et al. Sacramento area breast cancer epidemiology study: use of postmastectomy breast reconstruction along the rural-to-urban continuum. Plast Reconstr Surg 2010;126:1815-24. [Crossref] [PubMed]
- Morrow M, Mujahid M, Lantz PM, et al. Correlates of breast reconstruction: results from a population-based study. Cancer 2005;104:2340-6. [Crossref] [PubMed]
- Alderman AK, Hawley ST, Janz NK, et al. Racial and ethnic disparities in the use of postmastectomy breast reconstruction: results from a population- based study. J Clin Oncol 2009;27:5325-30. [Crossref] [PubMed]
- Butler PD, Familusi O, Serletti JM, et al. Influence of race, insurance status, and geographic access to plastic surgeons on immediate breast reconstruction rates. Am J Surg 2018;215:987-94. [Crossref] [PubMed]
- Soni SE, Lee MC, Gwede CK. Disparities in Use and Access to Postmastectomy Breast Reconstruction Among African American Women: A Targeted Review of the Literature. Cancer Control 2017;24:1073274817729053. [Crossref] [PubMed]
- Sharma K, Grant DW, Myckatyn TM. The Impact of Race on Choice of Post-Mastectomy Reconstruction: Is There a Healthcare Disparity? Plast Reconstr Surg 2015;136:114-5. [Crossref]
- Shippee TP, Kozhimannil KB, Rowan K, et al. Health insurance coverage and racial disparities in breast reconstruction after mastectomy. Womens Health Issues 2014;24:e261-9. [Crossref] [PubMed]
- Yang RL, Newman AS, Reinke CE, et al. Racial disparities in immediate breast reconstruction after mastectomy: impact of state and federal health policy changes. Ann Surg Oncol 2013;20:399-406. [Crossref] [PubMed]
- DeCoster RC, Stout MA, Burns JC, et al. Appalachian Status Is a Negative Predictor of Breast Reconstruction Following Breast Cancer Resection. Ann Plast Surg 2019;83:e15-9. [Crossref] [PubMed]
- Anderson SR, Sieffert MR, Talarczyk CMR, et al. Geographic Variation in Breast Reconstruction Modality Use Among Women Undergoing Mastectomy. Ann Plast Surg 2019;82:382-5. [Crossref] [PubMed]
- DeCoster RC, Bautista RF Jr, Burns JC, et al. Rural-Urban Differences in Breast Reconstruction Utilization Following Oncologic Resection. J Rural Health 2020;36:347-54. [Crossref] [PubMed]
- Bauder AR, Gross CP, Killelea BK, et al. The Relationship Between Geographic Access to Plastic Surgeons and Breast Reconstruction Rates Among Women Undergoing Mastectomy for Cancer. Ann Plast Surg 2017;78:324-9. [Crossref] [PubMed]
- Roughton MC, DiEgidio P, Zhou L, et al. Distance to a Plastic Surgeon and Type of Insurance Plan Are Independently Predictive of Postmastectomy Breast Reconstruction. Plast Reconstr Surg 2016;138:203e-11e. [Crossref] [PubMed]
- Albornoz CR, Cohen WA, Razdan SN, et al. The Impact of Travel Distance on Breast Reconstruction in the United States. Plast Reconstr Surg 2016;137:12-8. [Crossref] [PubMed]
- Bauder AR, Sarik JR, Butler PD, et al. Geographic Variation in Access to Plastic Surgeons. Ann Plast Surg 2016;76:238-43. [Crossref] [PubMed]
- Eom JS, Kobayashi MR, Paydar K, et al. The number of operations required for completing breast reconstruction. Plast Reconstr Surg Glob Open 2014;2:e242. [Crossref] [PubMed]
- Anonymous (2019). United States Department of Housing and Urban Development. Quick Facts Vermont.
- Dasari CR, Gunther S, Wisner DH, et al. Rise in microsurgical free-flap breast reconstruction in academic medical practices. Ann Plast Surg 2015;74:S62-5. [Crossref] [PubMed]
- Greenberg CC, Lipsitz SR, Hughes ME, et al. Institutional variation in the surgical treatment of breast cancer: a study of the NCCN. Ann Surg 2011;254:339-45. [Crossref] [PubMed]
- Nickel KB, Fox IK, Margenthaler JA, et al. Effect of Noninfectious Wound Complications after Mastectomy on Subsequent Surgical Procedures and Early Implant Loss. J Am Coll Surg 2016;222:844-852.e1. [Crossref] [PubMed]
- Spear SL, Hannan CM, Willey SC, et al. Nipple-sparing mastectomy. Plast Reconstr Surg 2009;123:1665-73. [Crossref] [PubMed]
- Roberts A, Baxter N, Camacho X, et al. Once is Rarely Enough: A Population-Based Study of Reoperations after Postmastectomy Breast Reconstruction. Ann Surg Oncol 2015;22:3302-7. [Crossref] [PubMed]
- Rubino C, Figus A, Lorettu L, et al. Post-mastectomy reconstruction: a comparative analysis on psychosocial and psychopathological outcomes. J Plast Reconstr Aesthet Surg 2007;60:509-18. [Crossref] [PubMed]
- Odom EB, Sharma K, Grant DW, et al. A Retrospective Cohort Study on Payor Type and the Effect on Revisions in Breast Reconstruction. Plast Reconstr Surg 2017;140:527e-37e. [Crossref] [PubMed]
- Orr JP, Sergesketter AR, Shammas RL, et al. Assessing the Relationship between Anxiety and Revision Surgery following Autologous Breast Reconstruction. Plast Reconstr Surg 2019;144:24-33. [Crossref] [PubMed]
- Bennett KG, Qi J, Kim HM, et al. Association of Fat Grafting With Patient-Reported Outcomes in Postmastectomy Breast Reconstruction. JAMA Surg 2017;152:944-50. [Crossref] [PubMed]
- Weichman KE, Broer PN, Thanik VD, et al. Patient-Reported Satisfaction and Quality of Life following Breast Reconstruction in Thin Patients: A Comparison between Microsurgical and Prosthetic Implant Recipients. Plast Reconstr Surg 2015;136:213-20. [Crossref] [PubMed]
- Pusic AL, Matros E, Fine N, et al. Patient-Reported Outcomes 1 Year After Immediate Breast Reconstruction: Results of the Mastectomy Reconstruction Outcomes Consortium Study. J Clin Oncol 2017;35:2499-506. [Crossref] [PubMed]
- Vyas KS, Hambrick HR, Shakir A, et al. A Systematic Review of the Use of Telemedicine in Plastic and Reconstructive Surgery and Dermatology. Ann Plast Surg 2017;78:736-68. [Crossref] [PubMed]
- Gfrerer L, Eberlin KR, Figura L, et al. Telemedicine and Plastic Surgery: Principles from the American Society of Plastic Surgeons Health Policy Committee. Plast Reconstr Surg 2022;150:221e-6e. [Crossref] [PubMed]
- Saad NH, AlQattan HT, Ochoa O, et al. Telemedicine and Plastic and Reconstructive Surgery: Lessons from the COVID-19 Pandemic and Directions for the Future. Plast Reconstr Surg 2020;146:680e-3e. [Crossref] [PubMed]
- Tam AK, Kim M, Mathew PJ, et al. The Doctor Will "See" You Now - Unmet Expectations of Telemedicine in Plastic Surgery. J Craniofac Surg 2021;32:1595-9. [Crossref] [PubMed]
Cite this article as: Silverstein ML, Nesbit RD, Collins MS, Willson TD. The impact of geographical access challenges on outcomes of postmastectomy breast reconstruction. Ann Breast Surg 2023;7:34.

