Combined localization technique with radio-guided occult lesion localization and Magseed for breast-conserving surgery for non-palpable multifocal breast cancer: a case report
Introduction
With increasing awareness of breast cancer in public and availability of breast imaging, breast cancers are diagnosed in earlier stage. Breast conservation therapy (BCT) is the treatment of choice for early cancer and the oncological safety had been confirmed by multiple randomized trial showing an equivalent disease-free and overall survival when compared with mastectomy (1-4). Some studies even show better survival in breast conserving group (5,6). However, in case of small, non-palpable lesion, this represents a unique challenge for the surgeon to localize the lesion accurately. Traditionally, wire guided localization (WGL) and radio-occult lesion localization (ROLL) are two commonly used adjuvants to localize the tumor during surgery. Each method has its own strengths and limitations (7). By inserting a wire to the tumor percutaneously, WGL can avoid the usage of radioactive substance. However, it limits the scheduling of procedure, carrying risk of wire complication, creating patient discomfort and hindering the cosmesis due to suboptimal surgical incision. Being a wireless procedure, ROLL can avoid the complications associated with the presence of wires but the use of radioactive substance usage has issues in safety precaution and radiation exposure (8). Therefore, there are different radiation-free wireless localization methods such as magnetic seed, radiofrequency tag and radar identification system invented in the past decade.
Multifocal breast cancer is not an absolute contraindication for BCT. However, the surgery is challenging as all of the foci have to be localized precisely, followed by en-bloc resection with a negative margin, particularly if the lesions are not palpable on clinical examination. From the literature, there are only scanty case reports reporting the use of ROLL for excision of multifocal non palpable breast cancer (9,10) and there might be interference of the signal from different injection foci causing inaccurate measurement. With an extensive choices of wireless localization methods nowadays, we reported a case of using two different technologies to aid the surgical resection of a multifocal non-palpable breast cancer. We present the following case in accordance with the CARE reporting checklist (available at https://abs.amegroups.com/article/view/10.21037/abs-22-20/rc).
Case presentation
A 53-year-old woman with no past medical history presented to us with two suspicious lesions identified on routine screening breast imaging. Clinically, there were no palpable mass in both breasts. She did not report any family history of breast cancer. On ultrasonography of her right breast, there was an 8-mm lesion identified in the lower inner quadrant of the right breast at the 4 o’clock position 5 cm from the nipple. Radiologically, it was of moderate suspicion of malignancy [Breast Imaging Report and Data System (BIRADS) 4b] and ultrasound- guided core biopsies were obtained from this lesion. In addition, there was another 6mm mildly suspicious lesion at the 3 o’clock position 6 cm from the nipple, radiologically graded as BIRADS 4a and core biopsies were also obtained from this lesion. The distance between the 2 foci is around 3 cm measured on ultrasonography. There was no abnormality detected on mammography. The pathology of these two lesions showed invasive ductal carcinoma. Contrast enhanced magnetic resonance imaging (MRI) was performed to identify potential occult lesions, but revealed no further lesions.
Pros and cons of BCT and mastectomy were discussed with the patient and she is very keen to preserve her breast. Hence, wide local excision together with sentinel lymph node biopsy, followed by V-mammoplasty were arranged. As the two lesions were not palpable on examination, they were localized pre-operatively by ROLL and magnetic seed marker (Magseed) insertion.
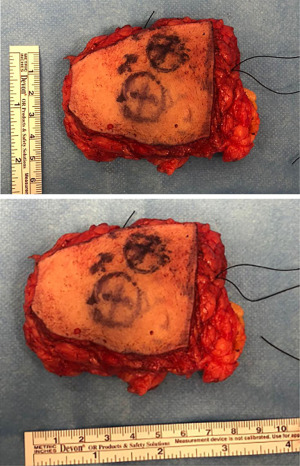
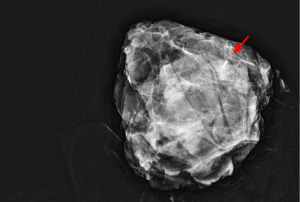
On the day of surgery, 0.3 mL of Tc99m sulphur colloid was injected into the center of the lesion at the 3 o’clock position while Magseed was inserted into the center of the lesion at 4 o’clock position under ultrasound guidance. Intraoperatively, the location of the 2 tumor foci were identified and marked as shown in Figure 1. Patent blue was also injected subcutaneously at the periareolar region and sentinel lymph node biopsy was performed with the aid of dual tracers technique. Subsequently, en-bloc wide local excision of the tumors was performed with the guidance of gamma probe and Sentimag probe. The size of the specimen measured 5 cm × 8 cm and it was shown in Figure 2. There were no residual radioactivity and magnetic field signal detected in the surgical field and specimen mammogram also confirmed inclusion of the Magseed with adequate margin as shown in Figure 3. For the defect at the lower-inner quadrant, it was reconstructed by V-mammoplasty. The post-operative clinical photo of the patient at the sitting position is shown in Figure 4. Although the right breast is slighter smaller compared to the non-operative side after the operation, the inframammary incision is well hidden and the shape are symmetrical on both sides. Pathological examination of the specimen confirmed the presence of two foci of invasive ductal carcinoma, measured 11 and 7 mm in diameter. The main foci were closest to the inferior margin by 8 mm and it was more than 1 cm from other resection margin. There was also high-grade ductal carcinoma in situ component found in the adjacent areas. During the clinic follow-up, our patient reported a high degree of satisfaction on the cosmetic result.

All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
In our knowledge, this is the first reported case that had utilized two different wireless localization techniques to manage multifocal non-palpable breast cancer.
WGL was considered as a gold standard for localizing non-palpable breast lesion since 1970s (11,12). However, in addition to patient discomfort, the presence of a wire is associated with various technical issues such as wire migration, wire breakage and wire transection. Furthermore, it also limits the choices of skin incision, significantly affecting the cosmetic outcome particularly in the era of modern oncoplastic surgery.
ROLL is the first non-wire localization technique invented in 1996 by European Institute of Oncology, Milan. By injecting a small dose (0.2–0.5 mCi) of sulfur colloid radio-labelled with 99m-Techneitum intratumorally 4–6 hours before the operation, the tumor can be localized intraoperatively with the aid of a hand-held gamma probe (13). There were few studies comparing ROLL versus WGL in the literature and they showed that there was no significant difference in the duration and difficulty on the radiological and surgical procedure with a comparable compete excision rate (14-17). More importantly, the radio-labelled colloid will travel along the lymphatic channel and accumulate in the axillary lymph node, allowing simultaneous sentinel lymph node biopsy—sentinel node and occult lesion localization (SNOLL).
In our case, there were two non-palpable tumor foci at the lower-inner quadrant of the right breast. BCT requires precise localization of the two lesions followed by a wide local excision with a clear margin. V-mammoplasty can be performed to reconstruct the defect after excision of the tumor at the lower-inner quadrant of the breast with supreme cosmesis (18). However, this requires extensive mobilization of the lateral breast parenchyma along a long inframammary incision. Therefore, a total wire-free localization technique is needed to facilitate the procedure. Assarian A reported a case of using ROLL for excision of non-palpable multicentric breast cancer in 2016 (9). There were two non-palpable tumor deposits located at the upper inner quadrant (10 o’clock) and upper outer quadrant (3 o’clock) of the left breast. Radioactive colloid was injected into the center of the two lesions and the locations were precisely identified by a gamma probe. In contrast, the two tumors in our patient were located closely with a distance of around 3 cm. In order to avoid the interference emitted from another lesion, localization utilizing two different signals are required. Magnetic seed localization is another wireless localization method that was first approved in US in 2016. Instead of injecting radioactive colloid, a tiny metal seed (Magseed) of a size of 5 mm is implanted directly into the center of the tumor under image-guidance. It is a permanent marker and the operation can be scheduled at any time after implantation, providing extra flexibility to the surgeons. With the aid of a specialized detection probe, the magnetic field signal emitted from Magseed can be precisely localized intraoperatively (19). With the help of ROLL and Magseed localization, the two tumor foci can be localized precisely without any signal interference from each other.
Breast cancer has become the most common cancer affecting women in Hong Kong since 1994. Due to the increase in awareness of the disease, more cases are diagnosed in the early stage by screening mammography or breast ultrasonography. Breast conserving surgery provide an alternative to mastectomy with a comparable oncological outcome but better cosmesis. Over the past two decades, different techniques had been developed to facilitate the excision of non-palpable tumor, from initially wire-guide localization to wireless, radiation free marker including magnetic seed, radiofrequency tag and radar localization system. Together with the mature oncoplastic surgery, patients’ satisfaction on the surgical treatment of breast cancer has been improved dramatically.
In conclusion, ROLL and magnetic seed localization can be used simultaneously for localizing different non-palpable breast tumor foci. A total wireless technique reduces patient discomfort and facilitate surgical excision.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://abs.amegroups.com/article/view/10.21037/abs-22-20/rc
Peer Review File: Available at https://abs.amegroups.com/article/view/10.21037/abs-22-20/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://abs.amegroups.com/article/view/10.21037/abs-22-20/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Veronesi U, Cascinelli N, Mariani L, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med 2002;347:1227-32. [Crossref] [PubMed]
- Blichert-Toft M, Nielsen M, Düring M, et al. Long-term results of breast conserving surgery vs. mastectomy for early stage invasive breast cancer: 20-year follow-up of the Danish randomized DBCG-82TM protocol. Acta Oncol 2008;47:672-81. [Crossref] [PubMed]
- Litière S, Werutsky G, Fentiman IS, et al. Breast conserving therapy versus mastectomy for stage I-II breast cancer: 20 year follow-up of the EORTC 10801 phase 3 randomised trial. Lancet Oncol 2012;13:412-9. [Crossref] [PubMed]
- Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med 2002;347:1233-41. [Crossref] [PubMed]
- van Maaren MC, de Munck L, de Bock GH, et al. 10 year survival after breast-conserving surgery plus radiotherapy compared with mastectomy in early breast cancer in the Netherlands: a population-based study. Lancet Oncol 2016;17:1158-70. [Crossref] [PubMed]
- Agarwal S, Pappas L, Neumayer L, et al. Effect of breast conservation therapy vs mastectomy on disease-specific survival for early-stage breast cancer. JAMA Surg 2014;149:267-74. [Crossref] [PubMed]
- Langhans L, Tvedskov TF, Klausen TL, et al. Radioactive Seed Localization or Wire-guided Localization of Nonpalpable Invasive and In Situ Breast Cancer: A Randomized, Multicenter, Open-label Trial. Ann Surg 2017;266:29-35. [Crossref] [PubMed]
- Cheang E, Ha R, Thornton CM, et al. Innovations in image-guided preoperative breast lesion localization. Br J Radiol 2018;91:20170740. [Crossref] [PubMed]
- Assarian A, Zand S. Radioguided Occult Lesion Localisation (ROLL) for Excision of Non-Palpable Breast Lesions, a Personal Experience in a Patient with Multifocal Breast Cancer. Arch Breast Cancer 2016;3:139-43.
- Paredes P, Vidal-Sicart S, Santamaría G, et al. Application of the ROLL technique in a case of bilateral multifocal breast cancer. Rev Esp Med Nucl 2008;27:436-9. [Crossref] [PubMed]
- Hall FM, Kopans DB, Sadowsky NL, et al. Development of wire localization for occult breast lesions: Boston remembrances. Radiology 2013;268:622-7. [Crossref] [PubMed]
- Perry NMEUSOMA Working Party. Quality assurance in the diagnosis of breast disease. EUSOMA Working Party. Eur J Cancer 2001;37:159-72. [Crossref] [PubMed]
- Belloni E, Canevari C, Panizza P, et al. Nonpalpable breast lesions: preoperative radiological guidance in radioguided occult lesion localisation (ROLL). Radiol Med 2011;116:564-74. [Crossref] [PubMed]
- van der Ploeg IM, Hobbelink M, van den Bosch MA, et al. 'Radioguided occult lesion localisation' (ROLL) for non-palpable breast lesions: a review of the relevant literature. Eur J Surg Oncol 2008;34:1-5. [Crossref] [PubMed]
- van Esser S, Hobbelink MG, Peeters PH, et al. The efficacy of 'radio guided occult lesion localization' (ROLL) versus 'wire-guided localization' (WGL) in breast conserving surgery for non-palpable breast cancer: a randomized clinical trial - ROLL study. BMC Surg 2008;8:9. [Crossref] [PubMed]
- Chu TY, Lui CY, Hung WK, et al. Localisation of occult breast lesion: a comparative analysis of hookwire and radioguided procedures. Hong Kong Med J 2010;16:367-72. [PubMed]
- Duarte C, Bastidas F, de los Reyes A, et al. Randomized controlled clinical trial comparing radioguided occult lesion localization with wire-guided lesion localization to evaluate their efficacy and accuracy in the localization of nonpalpable breast lesions. Surgery 2016;159:1140-5. [Crossref] [PubMed]
- Clough KB, Oden S, Ihrai T, et al. Level 2 oncoplastic surgery for lower inner quadrant breast cancers: the LIQ-V mammoplasty. Ann Surg Oncol 2013;20:3847-54. [Crossref] [PubMed]
- Constantinidis F, Sakellariou S, Chang SL, et al. Wireless localisation of breast lesions with MagSeed. A radiological perspective of 300 cases. Br J Radiol 2022;95:20211241. [Crossref] [PubMed]
Cite this article as: Hung RKW, Ip HW, Tsoi VYK. Combined localization technique with radio-guided occult lesion localization and Magseed for breast-conserving surgery for non-palpable multifocal breast cancer: a case report. Ann Breast Surg 2023;7:40.