
Physician’s comfort level with observing ductal carcinoma in situ of the breast: a survey of breast specialists at accredited breast centers in the United States
Introduction
Recently, there has been considerable attention to the over-diagnosis and overtreatment of low-grade ductal carcinoma in situ (DCIS) lesions that may never progress to invasive cancer, as a result of breast cancer screening (1). Furthermore, it is estimated that <1% of patients with DCIS will develop metastatic disease and/or death from their disease (2). Because the natural history of DCIS has not been fully elucidated, the current standard of care for low-grade DCIS is aggressive locoregional control with surgical resection and possible radiation therapy. However, many clinicians and researchers have proposed that this treatment paradigm is overtreatment of DCIS and may not be necessary for all cases of DCIS (1,3).
Several large trials are examining the role of surgery and radiation therapy in the treatment of lower risk DCIS lesions. These trials all involve randomization of low-grade DCIS patients to observation versus standard treatment. The LORIS (Low Risk DCIS) trial is currently open in the United Kingdom and includes women with grade 1 to 2 DCIS (4,5). The LORD (Management of Low-Risk DCIS) trial from the Netherlands, which is now closed to accrual, includes women older than 45 who have nuclear grade 1 DCIS (6). The COMET (Comparison of Operative versus Monitoring and Endocrine Therapy) trial from the United States includes women 40 years or older who have grade I or grade II, estrogen receptor (ER) and/or progesterone receptor (PR) positive DCIS. In the COMET trial, women under active surveillance can also be treated with endocrine therapy per their physician’s discretion (7). Recruitment to LORIS and COMET are ongoing and results from all three of these trials are not expected for many years. Trials such as these that randomize patients to a surgical versus nonsurgical intervention typically face many challenges, as providers and patients are not able to be blinded to their treatment arm. Nonetheless, COMET has accrued over 600 patients.
Physicians play a crucial role in patient recruitment clinical trials. They are often the first person to introduce a clinical trial to eligible patients. To understand different breast specialist’s opinions on this paradigm shift to observe DCIS, we conducted a survey of physicians working at accredited breast centers across the country from 2018 to 2019. We assessed three different types of physician specialties that have the most contact with newly diagnosed breast cancer patients: surgeons, medical and radiation oncologists. We first assessed physician’s knowledge about local and distant recurrence rates of DCIS stratified by different types of surgeries. Next, we assessed physician’s opinions about observing DCIS and for which types of patients they would be comfortable observing. Lastly, we assessed physician opinions on putting patients on DCIS observation trials. We examined whether there were any physician demographic or knowledge factors associated with physician’s willingness to recruit patients to DCIS observation trials. Of note, this study was conducted prior to the COVID-19 pandemic and does not reflect physician opinions of observation of DCIS during the pandemic. We present the following article in accordance with the STROBE reporting checklist (available at https://abs.amegroups.com/article/view/10.21037/abs-22-1/rc).
Methods
Study design and participants
A multidisciplinary, physician-based cross-sectional survey was designed specifically for physicians working at accredited hospitals and cancer centers by the National Accreditation Program for Breast Centers (NAPBC). NAPBC accredited programs have site-visit approved well-functioning multidisciplinary teams and have shown to provide superior care to non-accredited programs (8). The survey was distributed to NAPBC-accredited centers from 2018 to 2019, and if completed, would fulfill 1 of 2 annual quality improvement (QI) projects that was required (as per Standard 6.1, https://www.facs.org/quality-programs/napbc) for accreditation. In order to have a balanced composition of physician specialties, the respondents’ instructions stipulated that each NAPBC center had to return the completed survey from one of each of the following physician subspecialties that take care of patients with breast cancer: medical oncology, radiation oncology, and surgery (general or surgical oncology). All duplicate surveys were excluded. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Institutional Review Board of NorthShore University Health System (No. IRB17-0497) and individual consent for this study was waived.
Response rate
The survey was distributed to all NAPBC breast centers across the United States that were accredited at the time of initiating this study (n=603). Physician response rates were calculated by multiplying the number of centers by the required number of physician surveys per center (2 × number of centers) for the denominator, and total surveys returned minus duplicate surveys for the numerator. Facility response was calculated as the number of centers that participated in the survey divided by the total number of centers the survey was sent to. Duplicated surveys or surveys missing over 50% of responses were excluded from the analysis.
Development of the survey
Question topics were initially developed by investigators and then beta-tested through the University of Chicago Survey Lab who conducted conversational interviews with three surgeons, one medical oncologist and one radiation oncologist about the survey questions. The survey then consisted of an 11-item ad hoc questionnaire that covers physician opinions, observation of DCIS, reasons to not observe DCIS and comfort level in observing DCIS (see supplemental material for a copy of the survey, available at: https://cdn.amegroups.cn/static/public/abs-22-1-1.pdf).
Physician and facility characteristics
Self-reported data from each physician on specialty, gender, age, years in practice and number of patients with breast disease seen per week was collected. Location of physician practice was aggregated into Northeast, Midwest, South and West regions of the country and annual case load and type of center (free standing, hospital based, group practice). Affiliation with a medical school was recorded for each facility.
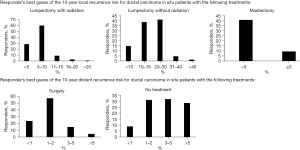
Physician knowledge of recurrence rates with DCIS
Physicians were asked to give their best estimate of local recurrence of DCIS with breast conserving therapy (BCS) alone, BCS plus radiation, or mastectomy, and distant recurrence risk with or without surgery (five questions total). Correct answers for the local recurrence risk (LRR) at 10 years for lumpectomy with radiation was 5–10%; LRR at 10 years for lumpectomy without radiation was 20–30%, LRR at 10 years after mastectomy was <5% and distant recurrence risk 1–2% with surgery. A composite score was collected including all the aforementioned knowledge questions except knowledge regarding the 10-year distant recurrence risk for DCIS patients with no treatment since literature on this risk is lacking. Knowledge was classified as a composite score such that “high” knowledge was defined as answering three or four out of four questions correctly and “low” knowledge as zero to two questions answered correctly.
Physician opinions
To gauge physician opinion on their comfort level with observing DCIS, physicians were asked to estimate the proportion of their patients they feel would qualify for observation and the level of evidence to support observation of DCIS (strong, moderate, weak/limited and no evidence). Physicians were asked about their comfort level (comfortable, neutral, uncomfortable) in observing different case scenarios of DCIS (low/high grade, ER positive/negative, >70 years old with high- or low-grade DCIS, >3 cm, <40 years old). Physicians were asked how easy or difficult it would be to put patients on a DCIS observation trial and reasons why they would not participate in a DCIS observation trial.
Statistical analysis
Survey responses were summarized using descriptive statistics. Physician knowledge was treated as a composite score of “high” knowledge and “low” knowledge defined by the number of correct answers to questions about DCIS recurrence rates. A multivariable logistic regression model adjusting for physician age, gender, specialty type, number of breast patients seen per week and years in practice and physician knowledge, was conducted to examine factors associated with higher composite knowledge about DCIS recurrence. A model incorporating the same aforementioned demographic and knowledge factors was conducted to assess factors associated with physician opinion on how easy it would be to put a DCIS patient on a clinical trial of observation. Missing data were excluded from analysis. All statistical analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC, USA). A P value <0.05 was considered statistically significant.
Results
There were 379 out of 603 (63%) NAPBC centers that participated in the study, with 979 out of 1,761 (56%) of physicians responding to the survey.
Demographic data
The demographic data of the responders are listed in Table 1. Approximately 51% of the responders were <50 years old, and 51.5% of the responders were female. Three hundred (32%) were medical oncologists, 316 (33.7%) were radiation oncologists, and 322 (34.3%) were surgeons.
Table 1
| Demographics | No. | % |
|---|---|---|
| Physicians (N=968) | ||
| Age (years) | ||
| 30–39 | 161 | 17.9 |
| 40–49 | 299 | 33.2 |
| 50–59 | 270 | 30.0 |
| ≥60 | 171 | 19.0 |
| Gender | ||
| Female | 478 | 51.5 |
| Male | 450 | 48.5 |
| Physician type | ||
| Breast surgeon | 322 | 34.3 |
| Medical oncologist | 300 | 32.0 |
| Radiation oncologist | 316 | 33.7 |
| Number of years in practice | ||
| <5 | 127 | 13.7 |
| 5–9 | 156 | 16.8 |
| 10–15 | 187 | 20.2 |
| 16–20 | 133 | 14.3 |
| >20 | 325 | 35.0 |
| Number of breast patients seen per week | ||
| <10 | 226 | 24.3 |
| 10–29 | 347 | 37.3 |
| 30–49 | 175 | 18.8 |
| ≥50 | 182 | 19.6 |
| NAPBC centers (N=379) | ||
| Center type | ||
| Free-Standing | 5 | 3.3 |
| Free-Standing with Hospital Affiliation | 26 | 17.0 |
| Group Practice | 6 | 3.9 |
| Hospital Based | 114 | 74.5 |
| Affiliated with a medical school | 46 | 12.1 |
| Region | ||
| Northeast | 86 | 22.7 |
| Midwest | 120 | 32.7 |
| South | 121 | 31.9 |
| West | 51 | 13.5 |
| International | 1 | 0.3 |
| Annual number of breast cancer cases | ||
| 0–300 | 145 | 68.1 |
| 301–600 | 41 | 19.3 |
| >600 | 27 | 13.0 |
NAPBC, National Accreditation Program for Breast Centers; No., number; %, proportion of physicians who chose the response.
Physician knowledge of recurrence rates with DCIS
Physicians were asked to estimate local and distant recurrence risks of DCIS by surgery type (Figure 1). There were 301 (31.1%) physicians who were categorized into the high knowledge group and 643 (66.4%) physicians in the low knowledge group. Five hundred and fifty-four (59.6%), 380 (40.9%), and 755 (81.2%) physicians answered correctly questions about LRR at 10 years after lumpectomy with radiation, lumpectomy without radiation and mastectomy, respectively. Five hundred and twenty-six (56.9%) physicians correctly stated the distant recurrence risk would be 1–2% with surgery, while 256 (28.4%) stated it would be >5% without treatment. Knowledge about recurrence rates with and without surgery or radiation varied by physician type (Table S1). A knowledge question regarding the 10-year distant recurrence risk for DCIS patients with no treatment was not included when determining composite knowledge, as there has been no significant data on this in the literature. A multivariable model showed that physician type, years in practice and physician gender were associated with a higher knowledge level (Table S2).
Physician opinion on observation of DCIS
When asked what physicians call DCIS during their patient consultations, 727 (76.9%) physicians refer to it as “non-invasive cancer”, while 159 (16.8%) refer to it as “cancer”. Three hundred and eighty-three (41.1%) physicians felt that there was strong or moderate evidence to support observation of DCIS, 50 (55.8%) felt there was weak to limited evidence and 29 (3.1%) responded that there was no evidence. Physicians were asked what proportion of their DCIS patients could undergo initial observation with no surgery or radiation therapy (Table 2). Three hundred and fifty-seven (57.5%) physicians felt that less than 20% of their patients with DCIS could potentially be treated with initial observation. Physicians were then asked about their comfort level in initially observing different case scenarios of DCIS rather then immediately treating these patients (Table 3). Physicians felt most comfortable observing DCIS was low-grade DCIS (n=326, 35.24%), and they felt the most uncomfortable observing high-grade DCIS (n=906, 97.31%).
Table 2
| Survey question and responses | No. | % |
|---|---|---|
| Regardless of current protocols, for what proportion of your DCIS patients do you think initial observation has the potential to be as or more appropriate than immediate treatment | ||
| None | 81 | 13.0 |
| Less than 20% | 357 | 57.5 |
| 21–40% | 131 | 21.1 |
| 41–60% | 40 | 6.4 |
| >60% | 12 | 1.9 |
DCIS, ductal carcinoma in situ; No., number; %, proportion of physicians who chose the response.
Table 3
| Survey question and responses | No. | % |
|---|---|---|
| Please rate your comfort level in initially observing rather than immediately treating the following patients with DCIS | ||
| High-grade DCIS | ||
| Comfortable | 15 | 1.61 |
| Neutral | 10 | 1.07 |
| Uncomfortable | 906 | 97.31 |
| Low-grade DCIS | ||
| Comfortable | 326 | 35.24 |
| Neutral | 223 | 24.11 |
| Uncomfortable | 376 | 40.65 |
| Patient over 70 years old with high- or low-grade DCIS | ||
| Comfortable | 217 | 23.41 |
| Neutral | 261 | 28.16 |
| Uncomfortable | 449 | 48.44 |
| DCIS greater than 3 cm | ||
| Comfortable | 15 | 1.61 |
| Neutral | 51 | 5.48 |
| Uncomfortable | 865 | 92.91 |
| DCIS patient under 40 years old | ||
| Comfortable | 16 | 1.71 |
| Neutral | 21 | 2.25 |
| Uncomfortable | 896 | 96.03 |
| ER negative DCIS | ||
| Comfortable | 25 | 2.68 |
| Neutral | 91 | 9.76 |
| Uncomfortable | 816 | 87.55 |
| ER positive DCIS | ||
| Comfortable | 215 | 23.09 |
| Neutral | 287 | 30.83 |
| Uncomfortable | 429 | 46.08 |
DCIS, ductal carcinoma in situ; ER, estrogen receptor; No., number; %, proportion of physicians who chose the response.
Physician opinions on clinical trials of observation of DCIS
Seven hundred and forty-six (76.5%) physicians felt it would be somewhat to very difficult to recruit patients to a DCIS observation trial and 212 (22.1%) stated it would be very or fairly easy. Physicians were asked for reasons why they might not participate in a DCIS observation trial (Table 4). The highest proportion of physicians (n=540, 57.0%) felt that “high risk of disease progression” was the most important major reason to not participate in a DCIS observation trial.
Table 4
| Survey question and responses | No. | % |
|---|---|---|
| Below are reasons why some doctors would not likely participate in a clinical trial of initial observation for DCIS. Which of these are reasons you might choose not to participate? | ||
| High risk of disease progression | ||
| Major reason | 540 | 57.0 |
| Minor reason | 280 | 29.5 |
| Not a reason | 128 | 13.5 |
| Patients would not consent | ||
| Major reason | 401 | 42.6 |
| Minor reason | 325 | 34.5 |
| Not a reason | 215 | 22.8 |
| Unsure of how to explain active surveillance to patients | ||
| Major reason | 81 | 8.6 |
| Minor reason | 266 | 28.2 |
| Not a reason | 596 | 63.2 |
| Medical center would not support observation of DCIS | ||
| Major reason | 71 | 7.5 |
| Minor reason | 228 | 24.2 |
| Not a reason | 643 | 68.3 |
| Going against standard of care | ||
| Major reason | 286 | 30.1 |
| Minor reason | 333 | 35.1 |
| Not a reason | 330 | 34.8 |
| Worry about tumor upstaging seen with surgery | ||
| Major reason | 422 | 44.3 |
| Minor reason | 388 | 40.8 |
| Not a reason | 142 | 14.9 |
DCIS, ductal carcinoma in situ; No., number; %, proportion of physicians who chose the response.
A multivariable model adjusting for physician demographic factors and composite knowledge about DCIS recurrence rates did not find an association between any physician factors and physician opinion on how easy it would be to put DCIS patients on a clinical trial of observation (Table S3).
Discussion
This is the first study since randomized trials of DCIS observation were launched to examine physician opinions about observation of DCIS and recruitment to clinical DCIS observation trials. The majority of physicians stated that about a fifth of their patients could be observed and that it would be difficult to recruit patients to a DCIS observation study. Unfortunately, we were not able to identify any actionable physician or knowledge factor that could be modified in the future to increase physician comfort level in putting patients on DCIS observation trials. However, our study does illustrate some interesting points about physician attitudes toward the observation of DCIS.
Physicians did report they were comfortable observing some cases of DCIS and most of these cases would have partially qualified for inclusion criteria for the COMET trial; however, we did not specify combinations of these factors which are required to enroll into COMET. Approximately a third of physicians felt comfortable observing low-grade DCIS and a quarter felt comfortable observing ER positive disease. These are both criteria for eligibility for the COMET trial. Physicians were aligned with factors that would exclude a patient from the COMET trial; over 85% of physicians were not comfortable observing either high-grade DCIS, DCIS in a young woman or ER negative DCIS, which are all exclusion criteria for the COMET trial. However, over 90% of physicians were not comfortable observing DCIS larger than 3 cm, but size is not necessarily an exclusion factor for participation in the COMET provided the entire area has been properly sampled.
Although knowledge was not independently associated with physician opinion on how easy it would be to put patients on a clinical trial, our study did show some knowledge deficits regarding DCIS recurrence rates. Nearly 20% of physicians responded that the LRR after mastectomy for DCIS was >5%, but several large studies and meta-analyses have demonstrated that the LRR is ~1% (9,10). Nearly a third of physicians answered that the distant recurrence risk of DCIS was >5% with no treatment. However, recent studies have shown low distant recurrence risks with DCIS. A retrospective review of patients with DCIS in the National Cancer Institute Surveillance, Epidemiology, and End Results (SEER) database, the 10-year breast cancer-specific survival for patients with low-grade DCIS was essentially the same between those who had surgery and those who did not (P value =0.95) (11). Surgeons and radiation oncologists had higher knowledge scores then medical oncologists despite adjusting for demographic factors, but it is not clear why we saw this finding.
The main reason survey responders selected to not participate on a clinical trial of observation of DCIS was worry about disease progression. Recent data on how many observed DCIS cases will progress to invasive disease is scant and may explain why physicians are worried about tumor progression. A study from 1995 and updated in 2005 demonstrated that 11 out of 28 women with low-grade DCIS that underwent biopsy alone eventually developed invasive cancer with 30-year follow-up (12,13). A Nurses Health Study from 2005 showed that those with DCIS that was not treated beyond the diagnostic biopsy were 13 times more likely to develop invasive cancer then those with non-proliferative disease regardless of grade of the DCIS (14). Many of the current DCIS observation trials, including the COMET trial, have strict inclusion criteria that may be less likely to be associated with disease progression that were not included in some of the aforementioned studies such as mammographic and biopsy criteria, ER positive disease or absence of microinvasion. One large study suggests that an increase in the development of invasion may occur with delays in treatment but this study included all types of DCIS, not the selected group of patients who are candidates for the DCIS observation trials (15). A more recent analysis of SEER found that patients with DCIS who were greater than 70 years old did not have a decreased future risk of invasive cancer when they were treated with surgery or surgery with radiation, compared to those not who had no local treatment (16). Models have shown that the progression of DCIS to invasive breast cancer may not be linear, and that only 14% to 50% of untreated DCIS lesions will progress to invasive cancer (17). Indeed, it has been suggested by some to define low-grade DCIS as an indolent lesion that behaves more like atypia (1,18). A recent study of 59 DCIS cases that were observed for 6 months on letrozole showed that 10% had invasive disease at resection but 15% had no residual DCIS. This may suggest that some DCIS lesions will respond to hormonal therapy alone and not require surgery (19). Patients on the COMET trial who are observed are given hormonal therapy, so it remains to be seen if this trial will show similar low disease progression rates as the aforementioned study. Furthermore, ongoing DCIS observation trials will determine which DCIS factors are associated with a low risk of tumor progression and which patients can safely be observed for the time period of the trial.
Another major concern of observing DCIS was tumor upstaging of DCIS lesions seen at surgical excision. Several studies have shown tumor upstaging rates of 8% to as high as 59%, with the average around 26% (20-22). A meta-analysis in 2011 of 52 studies and 7,350 DCIS cases showed a tumor upstage rate of 26% (23). The majority of these tumors are upstaged to small invasive cancers and factors associated with upstaging are exclusion criteria for DCIS observation trials such as COMET (23). One recent study that examined tumor upstage rates of patients who qualitied for the COMET, LORIS and LORD trials showed upstage rates of only 6–10% whereas another study showed upstage rates of 20% for patients qualifying for the LORIS trial (24,25). Many studies have demonstrated certain factors that can help physicians anticipate which DCIS tumors may be upstaged. Several studies have demonstrated that a palpable mass, larger size of lesion (>2 cm) and higher grade were associated with increased risk of upstaging, along with physician suspicion (22,26). Jakub et al. developed a validated nomogram, which utilizes biopsy grade, palpable mass, multicentricity, and size to help predict which DCIS tumors have an increased risk of upstaging (27). In this model, tumor upstaging for DCIS lesions that fulfill inclusion criteria for COMET was low: 7.4–14% for low-grade DCIS and 12–14% for ER positive DCIS (22,27). Certainly, more sensitive factors such as imaging biomarkers or other biologic markers that can better predict tumor upstaging with DCIS are needed then relying purely on clinical factors.
There are limitations to our study. This survey is inherently observational and is subject to bias. While limiting the questions to encourage a higher response rate, we may not have other reasons for physician discomfort with observing DCIS that are not captured in this survey. In addition, the survey does not address patient attitudes toward participating in DCIS observation trials, which also can impact clinical trial recruitment. Just over 40% of physicians did report that patients not consenting to a DCIS observation trial was a major reason to not place a patient on trial.
During the start of the COVID-19 pandemic in the United States, a consortium of experts from several cancer focused organizations released guidelines for the triage and prioritization of the surgical and nonsurgical management of patients with invasive breast cancer and DCIS (28). Patients with DCIS were generally placed in the Priority C group, meaning that their surgery could be delayed until after the COVID-19 pandemic. It will be interesting to see the number and type (hormone status, grade, etc.) of DCIS cases that were delayed during this time, the impact of these delays, and if it will change physician opinions about observing DCIS in the future.
In conclusion, we have shown that physicians who treat breast cancer patients from different practice backgrounds have a certain comfort level for observing DCIS, although for only a select group of patients. The majority of physicians currently do not feel there is strong enough data to support observing DCIS. Concerns about tumor progression and tumor upstaging with DCIS observation remain paramount concerns amongst physicians and ongoing trials and future studies will need to address these issues to convince physicians that some DCIS cases can be safely observed. Efforts to increase physician knowledge about recurrence rates with DCIS are needed but may not necessarily change physician recruitment to DCIS observation trials.
Acknowledgments
This work was presented as a poster presentation at the 20th annual meeting of the American Society of Breast Surgeons on May 3rd, 2019 in Dallas, TX, USA.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://abs.amegroups.com/article/view/10.21037/abs-22-1/rc
Data Sharing Statement: Available at https://abs.amegroups.com/article/view/10.21037/abs-22-1/dss
Peer Review File: Available at https://abs.amegroups.com/article/view/10.21037/abs-22-1/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://abs.amegroups.com/article/view/10.21037/abs-22-1/coif). RJB is Chair of NAPBC (NAPBC is the accrediting body for the breast centers). MM is the Vice Chair of the NCCN breast panel, but this is not a conflict to this study. SK is Chair of NAPBC. KAY is Vice Chair of NAPBC and President of Chicago Surgical Society. The other authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Esserman LJ, Thompson IM, Reid B, et al. Addressing overdiagnosis and overtreatment in cancer: a prescription for change. Lancet Oncol 2014;15:e234-42. [Crossref] [PubMed]
- Groen EJ, Elshof LE, Visser LL, et al. Finding the balance between over- and under-treatment of ductal carcinoma in situ (DCIS). Breast 2017;31:274-83. [Crossref] [PubMed]
- Esserman L, Yau C. Rethinking the Standard for Ductal Carcinoma In Situ Treatment. JAMA Oncol 2015;1:881-3. [Crossref] [PubMed]
- Francis A, Thomas J, Fallowfield L, et al. Addressing overtreatment of screen detected DCIS; the LORIS trial. Eur J Cancer 2015;51:2296-303. [Crossref] [PubMed]
- Francis A, Fallowfield L, Rea D. The LORIS Trial: Addressing overtreatment of ductal carcinoma in situ. Clin Oncol (R Coll Radiol) 2015;27:6-8. [Crossref] [PubMed]
- Elshof LE, Tryfonidis K, Slaets L, et al. Feasibility of a prospective, randomised, open-label, international multicentre, phase III, non-inferiority trial to assess the safety of active surveillance for low risk ductal carcinoma in situ - The LORD study. Eur J Cancer 2015;51:1497-510. [Crossref] [PubMed]
- Hwang ES, Hyslop T, Lynch T, et al. The COMET (Comparison of Operative versus Monitoring and Endocrine Therapy) trial: a phase III randomised controlled clinical trial for low-risk ductal carcinoma in situ (DCIS). BMJ Open 2019;9:e026797. [Crossref] [PubMed]
- Miller ME, Bleicher RJ, Kaufman CS, et al. Impact of Breast Center Accreditation on Compliance with Breast Quality Performance Measures at Commission on Cancer-Accredited Centers. Ann Surg Oncol 2019;26:1202-11. [Crossref] [PubMed]
- Timbrell S, Al-Himdani S, Shaw O, et al. Comparison of Local Recurrence After Simple and Skin-Sparing Mastectomy Performed in Patients with Ductal Carcinoma In Situ. Ann Surg Oncol 2017;24:1071-6. [Crossref] [PubMed]
- Boyages J, Delaney G, Taylor R. Predictors of local recurrence after treatment of ductal carcinoma in situ: a meta-analysis. Cancer 1999;85:616-28. [Crossref] [PubMed]
- Sagara Y, Mallory MA, Wong S, et al. Survival Benefit of Breast Surgery for Low-Grade Ductal Carcinoma In Situ: A Population-Based Cohort Study. JAMA Surg 2015;150:739-45. Erratum in: JAMA Surg 2015 Aug;150(8):820. [Crossref] [PubMed]
- Page DL, Dupont WD, Rogers LW, et al. Continued local recurrence of carcinoma 15-25 years after a diagnosis of low grade ductal carcinoma in situ of the breast treated only by biopsy. Cancer 1995;76:1197-200. [Crossref] [PubMed]
- Sanders ME, Schuyler PA, Dupont WD, et al. The natural history of low-grade ductal carcinoma in situ of the breast in women treated by biopsy only revealed over 30 years of long-term follow-up. Cancer 2005;103:2481-4. [Crossref] [PubMed]
- Collins LC, Tamimi RM, Baer HJ, et al. Outcome of patients with ductal carcinoma in situ untreated after diagnostic biopsy: results from the Nurses' Health Study. Cancer 2005;103:1778-84. [Crossref] [PubMed]
- Ward WH, DeMora L, Handorf E, et al. Preoperative Delays in the Treatment of DCIS and the Associated Incidence of Invasive Breast Cancer. Ann Surg Oncol 2020;27:386-96. [Crossref] [PubMed]
- Sun SX, Suk R, Kuerer HM, et al. No Treatment Versus Partial Mastectomy Plus Radiation for Ductal Carcinoma In Situ. Ann Surg Oncol 2022;29:39-41. [Crossref] [PubMed]
- Kuerer HM, Albarracin CT, Yang WT, et al. Ductal carcinoma in situ: state of the science and roadmap to advance the field. J Clin Oncol 2009;27:279-88. [Crossref] [PubMed]
- Ozanne EM, Shieh Y, Barnes J, et al. Characterizing the impact of 25 years of DCIS treatment. Breast Cancer Res Treat 2011;129:165-73. [Crossref] [PubMed]
- Hwang ES, Hyslop T, Hendrix LH, et al. Phase II Single-Arm Study of Preoperative Letrozole for Estrogen Receptor-Positive Postmenopausal Ductal Carcinoma In Situ: CALGB 40903 (Alliance). J Clin Oncol 2020;38:1284-92. [Crossref] [PubMed]
- Podoll MB, Reisenbichler ES, Roland L, et al. Feasibility of the Less Is More Approach in Treating Low-Risk Ductal Carcinoma In Situ Diagnosed on Core Needle Biopsy: Ten-Year Review of Ductal Carcinoma In Situ Upgraded to Invasion at Surgery. Arch Pathol Lab Med 2018;142:1120-6. [Crossref] [PubMed]
- Munck F, Clausen EW, Balslev E, et al. Multicentre study of the risk of invasive cancer and use of sentinel node biopsy in women with a preoperative diagnosis of ductal carcinoma in situ. Br J Surg 2020;107:96-102. [Crossref] [PubMed]
- Sheaffer WW, Gray RJ, Wasif N, et al. Predictive factors of upstaging DCIS to invasive carcinoma in BCT vs mastectomy. Am J Surg 2019;217:1025-9. [Crossref] [PubMed]
- Brennan ME, Turner RM, Ciatto S, et al. Ductal carcinoma in situ at core-needle biopsy: meta-analysis of underestimation and predictors of invasive breast cancer. Radiology 2011;260:119-28. [Crossref] [PubMed]
- Grimm LJ, Ryser MD, Partridge AH, et al. Surgical Upstaging Rates for Vacuum Assisted Biopsy Proven DCIS: Implications for Active Surveillance Trials. Ann Surg Oncol 2017;24:3534-40. [Crossref] [PubMed]
- Pilewskie M, Stempel M, Rosenfeld H, et al. Do LORIS Trial Eligibility Criteria Identify a Ductal Carcinoma In Situ Patient Population at Low Risk of Upgrade to Invasive Carcinoma? Ann Surg Oncol 2016;23:3487-93. [Crossref] [PubMed]
- Si J, Yang B, Guo R, et al. Factors associated with upstaging in patients preoperatively diagnosed with ductal carcinoma in situ by core needle biopsy. Cancer Biol Med 2019;16:312-8. [Crossref] [PubMed]
- Jakub JW, Murphy BL, Gonzalez AB, et al. A Validated Nomogram to Predict Upstaging of Ductal Carcinoma in Situ to Invasive Disease. Ann Surg Oncol 2017;24:2915-24. [Crossref] [PubMed]
- Dietz JR, Moran MS, Isakoff SJ, et al. Recommendations for prioritization, treatment, and triage of breast cancer patients during the COVID-19 pandemic. the COVID-19 pandemic breast cancer consortium. Breast Cancer Res Treat 2020;181:487-97. [Crossref] [PubMed]
Cite this article as: Poli EC, Chang C, Bleicher RJ, Moran M, Dietz J, Sarantou T, Kurtzman S, Yao KA; Data Working Group National Accreditation Program for Breast Centers. Physician’s comfort level with observing ductal carcinoma in situ of the breast: a survey of breast specialists at accredited breast centers in the United States. Ann Breast Surg 2023;7:21.

