
The modified Wise-pattern superomedial pedicle reduction mammoplasty for benign macromastia: a 9-year case series
Introduction
Excessive breast tissue with physical and psychosocial symptoms is broadly termed macromastia. Those patients with macromastia requiring a reduction of greater than 1,500 grams per breast are generally considered to have gigantomastia, though there is no definite consensus. Gigantomastia has been characterized by etiology (1), percent contribution to body mass index (BMI), and grams of breast tissue per body surface area (BSA); the latter has been frequently used by insurance carriers to determine medical necessity (2) for breast reductions. Physical symptoms like neck, back, shoulder and arm pain, headaches, rashes, itching, upper extremity numbness, and bra strap grooving are often cited as reasons for seeking treatment (3). It is also known that psychosocial symptoms like anxiety, depression (4), diminished sexual function (5), poor self-image deeply affect macromastia patients. Unsurprisingly, the pervasive impact of breast hypertrophy on quality of life and lifestyle has made reduction mammoplasty commonplace, with 103,098 procedures performed in 2017 alone (6). A wide range of patients have enjoyed improvement in virtually every dimension, including quality of life, both in the short and long term after undergoing surgery (4).
According to the American Board of Plastic Surgery Maintenance of Certification dataset in 2014, 59% of the plastic surgeons used an inferior pedicle for reduction mammoplasty likely due to its vascular reliability (7,8). Despite recent evidence showing no significant difference in major or minor complication rates (9), regardless of the volume resected (10), surgeons routinely favoring the superomedial pedicle continue to be in the minority (7). Patients have reported increased long-term overall satisfaction, satisfaction with projection and contour of breasts (11), as well as shape and symmetry of breasts (12) in the superomedial pedicle cohort as compared to the inferior pedicle cohort.
Traditionally, it was thought that inferior pedicles reduced breast ptosis (13), but were associated with bottoming out (14,15). Consequently, Pitanguy et al. introduced the superomedial pedicle (16) which has not necessarily been shown to solve the problem of long-term nipple-areolar complex (NAC) displacement (12,17) likely because additional factors like volume of resection and parenchymal excision patterns confound comparisons across studies. Hall-Findlay recommended against excessive parenchymal excision cranial to the superomedial pedicle to prevent NAC retraction (18). The senior author of this paper has expanded on this concept and formally referred to the modification as the “superior-ledge superomedial pedicle” (SL-SMP) technique (19) Our analysis of 107 patients having undergone SL-SMP reduction mammoplasty over 5 years with a mean follow-up of 44.6 months found no incidence of clinically relevant NAC retraction. Thus, we prefer using the SL-SMP technique for its versatility and outcomes.
Two common incision patterns have been combined with a superomedial pedicle for reduction mammoplasty. Vertical pattern incisions offer a reduced scar burden but can be challenging to perform in gigantomastia. Wise pattern incisions can be utilized on almost any patient but require long scars and are prone to complications at the confluence of the horizonal and vertical suture lines, also known as the “T-junction” or “T-point”. The “inverted V” (IV) modification of has been described previously to address this problem (20). It has been shown to reduce the incidence of wound complications at the T-point, likely by decreasing tension at the site. Our group analyzed wound complications of 88 patients over 5 years, capturing both the pre and post implementation phases of the IV technique. We found a reduction in wound complications at the T-point from 18% to 6% (P=0.026) after implementation of the IV technique (21). Since then, we have incorporated the IV modification in reduction mammoplasties for benign macromastia.
The objective of this study is to provide an update with nearly a decade of experience employing the “inverted V” Wise-pattern superior-ledge superomedial pedicle (IV-SL-SMP) for reduction mammoplasty in benign macromastia. Additionally, we analyze the safety and efficacy of our techniques in specific high-risk patients including overweight/obese BMI, smokers, diabetics, and high resection weights. We present the following article in accordance with the TREND reporting checklist (available at https://abs.amegroups.com/article/view/10.21037/abs-21-102/rc).
Methods
The Institutional Review Board at New York Presbyterian/Columbia University Irving Medical Center approved this study under ID: IRB-AAAS1361 and individual consent was waived given the nature of the retrospective chart review. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
All patients who underwent reduction mammoplasty for benign macromastia or gigantomastia performed by the senior author (CHR) at Columbia University Medical Center between January 2010 and September 2018 were identified from a prospectively collected database and reviewed retrospectively. All patients with benign macromastia underwent a superomedial pedicle, Wise-pattern, superior ledge breast reduction with an inverted V pattern at the T-point.
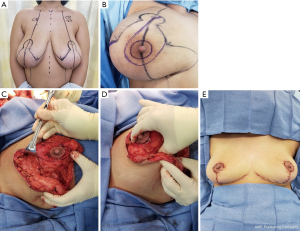
The IV-SL-SMP reduction mammoplasty involves two variations: (I) a full-thickness “inverted V” incision approximately 2 cm in width, at the junction of the breast meridian and inframammary fold; and (II) creation of a “superior ledge” which serves as the base of the NAC through the partial-thickness excision of tissue superolateral to the pedicle. Both techniques have been published (19,21). There have been no other significant modifications to the senior author’s (CHR) operative approach since May 2009. The technique is summarized in Figure 1.
Patients who underwent unilateral breast reduction or oncoplastic breast reduction were excluded from the study. Patient demographics, intraoperative data, and outcomes were gathered from the electronic medical record and coded into a HIPAA-compliant database at Columbia University Medical Center. Independent variables included age, BMI, diabetes status, smoking status, ASA classification, length of surgery, total weight of resection, and length of follow-up. Specific outcomes tracked included: reoperations/readmissions, surgical site infections (SSI), hematoma, seroma, prolonged wound healing, T-point wounds, nipple loss, loss of nipple sensation, fat necrosis, and need for revisional procedures. Any wound one centimeter or larger requiring dressing changes was classified as delayed wound healing. Clinic notes were carefully reviewed for each follow up visit for all patients. If any of the above findings were noted on physical exam of the surgical site, the patient was considered to have a complication, regardless of the time to resolution, treatment, number of notes documenting the abnormalities, or author of note. Patients without complications had normal exams documented in all notes.
Statistical analysis
Regression analyses were performed at the group level to determine whether the independent variables were associated with outcomes using Stata. Statistical significance was set at P<0.05.
Results
There were a total of 209 patients who underwent reduction mammoplasty during the study period. Of these patients, 148 underwent breast reduction for benign macromastia while the remaining 61 patients underwent oncoplastic breast reduction and were subsequently excluded from the analysis. Mean age of the cohort was 39.8 years and mean BMI was 29.6 kg/m2. Twenty-two patients (14.9%) were former smokers, 126 patients (85.1%) never smoked, and 9 patients (6.1%) were diabetics. ASA classifications were as follows: ASA 1, 39 patients (27.5%); ASA 2, 94 patients (66.2%); and ASA 3, 9 patients (6.3%). Mean length of anesthesia was 216.2 minutes, mean total resection weight was 1,623 grams, and mean follow-up length was 40.5 weeks from the date of the index surgery. Table 1 includes ranges for the relevant demographic data.
Table 1
| Characteristics | Value |
|---|---|
| Age (years), mean [range] | 39.8 [14–71] |
| BMI (kg/m2), mean [range] | 29.6 [19.2–44.5] |
| Smoking status, n (%) | |
| Never | 126 (85.1) |
| Former | 22 (14.9) |
| Current | 0 (0.0) |
| Diabetics, n (%) | 9 (6.1) |
| ASA grade, n (%) | |
| 1 | 39 (27.5) |
| 2 | 94 (66.2) |
| 3 | 9 (6.3) |
| Length of surgery (min), mean [range] | 216 [144–353] |
| Resection weight (g), mean [range] | 1,623 [307–5,419] |
| Follow-up (wk), mean [range] | 40.5 [2–269] |
N=148; mean age, BMI, length of surgery, resection weight, and follow-up reported. BMI, body mass index; kg/m2, kilograms per meter squared; ASA, American Society of Anesthesiologists; min, minutes; g, grams; wk, weeks.
Of the patients experiencing any complication (n=47, 31.8%), the most common complications were partial loss of nipple sensation (n=34, 23%), minor fat necrosis (n=25, 16.9%), and delayed wound healing (n=14, 9.5%). Most complications were treatable with local wound care, however a minority of patients (n=8, 5.4%) opted for revisional procedures for: fat grafting (n=3), glandular ptosis (n=1), “dog ear” revision (n=1), bottoming out (n=1), hypertrophic scarring (n=1), NAC tattooing (n=1). Of note, major complications (n=3, 1.9%) were limited to 2 patients requiring takebacks for postoperative hematomas and one readmission for noncardiac chest pain unrelated to the operation. No patients required operative treatment for infections or seromas. No patients experienced complete loss of sensation or complete necrosis of the nipple. Frequency of patients experiencing complications are listed in Table 2.
Table 2
| Complications | N (%) | Associated variable (P value)* |
|---|---|---|
| Major complications | 3 (2.0) | |
| Reoperation | 2 (1.3) | |
| Readmission | 1 (0.7) | |
| Surgical site infection | 9 (6.1) | |
| Delayed wound healing | 14 (9.5) | BMI (0.007) |
| T-point wound | 5 (3.4) | Total resection weight (0.043) |
| Hematoma | 3 (2.0) | |
| Seroma | 2 (1.4) | |
| Nipple loss | ||
| Partial | 2 (1.4) | |
| Full | 0 (0.0) | |
| Nipple sensation | Age (0.031) | |
| Partial | 34 (23.0) | |
| None | 0 (0.0) | |
| Fat necrosis | 25 (16.9) | |
| Revisional procedures | 8 (5.4) | |
| Any complication | 47 (31.8) |
N=148; ^, patients may have experienced more than 1 complication, therefore sum of percentages will not equal 100. *, only significantly associated (P<0.05) variables reported.
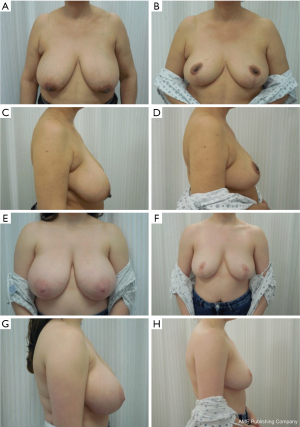
Age was significantly associated with loss of nipple sensation (P=0.031). BMI was significantly associated with delayed wound healing (P=0.007). Total resection weight was significantly associated with T-point wounds (P=0.043). There were no significant associations between the remaining independent variables (diabetes status, smoking status, ASA classification, length of surgery, follow up time) and reoperations/readmissions, SSI, hematoma, seroma, nipple loss, fat necrosis, and need for revisional procedures. Postoperative pictures can be seen in Figures 2,3.
Discussion
Several combinations of incisions and pedicles have been described to meet the goals of reduction mammoplasty which are to: (I) preserve vascularity and innervation to the nipple areolar complex (NAC), (II) perform appropriate volume reduction, (III) create a skin envelope that minimizes scarring and maintains proportionality to the remaining breast tissue, and (IV) maintain an aesthetic breast shape (22). The novel IV-SL-SMP reduction mammoplasty is a safe, efficacious operative strategy which meets these criteria.
Because we avoid separating the pedicle from the pectoralis fascia, the neurovascular supply to the flap and NAC are not disrupted by the IV-SL-SMP approach. Anatomical studies have demonstrated that a medial flap containing the perforator arteries arising from the internal thoracic artery is critical for viability of the NAC (23,24). Only 1.4% of our patients experienced partial necrosis of the NAC and 0% experienced complete NAC necrosis. According to Brownlee et al.’s systematic review, NAC necrosis occurred in 0–1.7% of patients who underwent inferomedial pedicles as compared to 0–4.3% in patients with a superomedial pedicle (10). Perhaps the preservation of the dermoglandular superior ledge in our technique confers a modest benefit in NAC necrosis relative to the traditional superomedial pedicle technique. Though the most common complication encountered was partial loss of nipple sensation (23% patients), no patient experienced complete loss of sensation over the follow up period (mean 40 weeks). In a small cohort on which the Hall-Findlay technique was employed, Swanson noted that 51% of patients experienced numbness of the NAC at 3.9 months and 10.6% of patients reported persistent partial sensation loss at the end of a 2 year follow up (25). In another study, the superomedial pedicle group experienced no significant difference in nipple sensation as compared to the inferomedial group (11% breasts vs. 13.5% breasts, P=0.61) over a minimum follow up of 3 months (10). Additional data on whether different pedicles result in permanent and clinically significant differences in NAC sensation is needed (23,26,27). We found that increasing age was significantly associated with risk of partial loss of nipple sensation which is consistent with other studies that have found age is associated with an increased risk of complications (28).
Concerns about the increased risk of complications in large resections with superomedial pedicles have been a barrier to widespread utilization in reduction mammoplasty (8,29-31). This notion has been addressed in multiple studies as superomedial pedicles have been safely and consistently used in cohorts with mean resection weights greater than 600 grams (9,10,30,32). Despite a mean resection weight of 1,623 grams in our cohort, our overall complication rate (31.8%) is in the low end of the range of what other groups have published (31.5–52%) while our major complication rate (2.0%) is less than previous case series (6.7–10.9%) (28,30,33-35). None of the patients in our cohort required reoperation for excision of additional tissue. This is clear evidence that superomedial pedicles adequately allow for large volume resections and carry a low risk.
There is an ongoing debate on whether a vertical incision or a Wise pattern incision offers a skin envelope with minimal scarring and wound complications. In a randomized controlled trial, Thoma et al. found no difference in health-related quality of life between patients in either group (36). Fernandez et al. further demonstrated that overall aesthetic scores were higher in patients with the inverted T scar, though authors noted that patient factors were more important than incision for a favorable aesthetic outcome (37). Wound complications were disproportionately responsible for 27–57% (Wise/inverted T group) vs. 21.7–44% (vertical scar group) of overall complications even if the aforementioned studies did not appreciate statistically significant differences in overall or wound complications (9,35,37). On the other hand, Young et al. reported a wound complication rate of 3.8% according to the NSQIP data, but noted that small wound healing problems may not have met the thresholds for the diagnosis of a complication in the database (38). This likely accounts for the variability in complication rates seen between institutional case series. Given the inconsistent definitions of “wound complications” in similar studies, we avoided reporting an overall wound complication rate in an effort to give a clearer profile of our outcomes to the readers. In our cohort, 9.5% of patients experienced delayed wound healing as compared to 10–22% in similar groups (8,29). A significant proportion of patients (7.5–34.6%) experience complications at the T-junction, prompting surgeons to investigate modifications which may reduce this burden (30,39,40). Though CHR had previously found that the IV technique reduced T-junction complications by two-thirds, 6% of overall patients were still affected. With the inverted V modification, we found that only 3.4% of our patients have experienced T-junction wound complications. Increased BMI and increased resection weight were associated with an increased risk of delayed wound healing and T-point wound complications, respectively, in our study. These associations, though seemingly intuitive, have not been consistently demonstrated (28). We surmise that the mechanism for the reduced complication rate of the “inverted V” lies in reducing tension at the triple point in the Wise pattern incision (21). It is important to note that the “inverted V” is still subject to tension at the triple point making it prone to breakdown and a scar that may be perceived as aesthetically inferior. Many patients who undergo a standard Wise pattern incision, however, have the T-junction pulled superiorly forming an “inverted V” anyway. Pincushion deformities and abnormal curvature of the inframammary fold are possible complications of the “inverted V” modification, though neither of these events were noted our chart review. Finally, a complete dehiscence at the triple point in a patient who has undergone the IV-SL-SMP modifications could theoretically take a substantial amount of time to re-epithelialize due to the de-epithelialization of the inferior pedicle inherent to technique described. No patients experienced a complete dehiscence in this cohort; wound complications in this area were limited to a slight epidermolysis that resolved with antibiotic ointment and dry dressing changes. Unfortunately, our chart review did not capture the exact length of time required for complete wound healing. Generally, wounds in this area healed from one postoperative visit to the next (approximately 2 weeks).
The SL-SMP technique helps maintain proportionality to the surrounding tissue and an aesthetic breast shape. The spiral rotation of the pedicle improves projection of the NAC and prevents ptosis. The parenchymal ledge on which the NAC rests minimizes ‘bottoming out’ and allows for a tension-free inset thereby promoting circumareolar healing. The ledge thickness is individualized to the patient accounting for the volume of resection and preferences for NAC projection. The rate of revisional procedures performed in our patients was on the lower end as compared to other groups which suggests that our patients are generally satisfied with results (10,28,29).
Reduction mammoplasty has been a successful intervention for macromastia by any measure. It carries complications that occur with variable frequency in the literature. Our rates of major complications (2.0%), unplanned reoperations (1.3%), and readmissions (0.7%) are slightly lower than what has been recently reported. In two analyses of primary breast reductions for noncancerous indications using the National Surgical Quality Improvement Program (NSQIP) database, a major complication rate of 2.0–3.0%, an unplanned reoperation rate of 1.4-1.9%, and a readmission rate of 1.1–1.4% was appreciated (38,41).
Limitations
Though this study demonstrates that the IV-SL-SMP approach is a safe, effective option that rivals other techniques for reduction mammoplasty, there are some significant limitations. This cohort is relatively small and was studied at a single site. Despite the standardization conferred by involving only one surgeon, generalizability due to surgeon preferences and organizational factors is limited. The location of our institution may predispose our study to a selection bias for patients with lower socioeconomic status and more comorbidities than the general population. Additionally, there were no pictures in the electronic medical record which forced outcomes to be coded based on written accounts of practitioners allowing for variability of data entry due to misinterpretation. CHR adopted the technique in 2010, thus, her learning curve may have had an impact on the results. Mean follow up time was 40 weeks which may not completely capture long-term results.
Conclusions
This study reports a nine-year experience with the IV-SL-SMP approach for reduction mammoplasty. Our results indicate that this modification is an acceptable approach with similar outcomes and no significant increase in morbidity for treatment of benign macromastia.
Acknowledgments
The authors would like to thank Dr. Roman Nowygrod, the Thomas C. King Surgical Education Fellowship at Columbia University Medical Center Department of Surgery, and Dr. Christine Rohde for providing time, guidance, and resources for this project. Abstract was previously presented at American Society of Plastic Surgeons: 88th Annual Plastic Surgery Meeting, September 20–23, 2019, San Diego Convention Center, San Diego, California, United States of America.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the TREND reporting checklist. Available at https://abs.amegroups.com/article/view/10.21037/abs-21-102/rc
Data Sharing Statement: Available at https://abs.amegroups.com/article/view/10.21037/abs-21-102/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://abs.amegroups.com/article/view/10.21037/abs-21-102/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The Institutional Review Board at New York Presbyterian/Columbia University Irving Medical Center approved this study under ID: IRB-AAAS1361 and individual consent was waived given the nature of the retrospective chart review.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Dancey A, Khan M, Dawson J, et al. Gigantomastia--a classification and review of the literature. J Plast Reconstr Aesthet Surg 2008;61:493-502. [Crossref] [PubMed]
- Koltz PF, Frey JD, Langstein HN. Insurance coverage and reduction mammaplasty: a systematic review of current health care policies. Plast Reconstr Surg 2013;132:692e-3e. [Crossref] [PubMed]
- American Society of Plastic Surgeons. ASPS Recommended Insurance Coverage Criteria for Third-Party Payers, Reduction Mammaplasty. Position Paper approved by the ASPS Board of Directors 2002. Available online: http://www.plasticsurgery.org/Documents/medical-professionals/health-policy/key-issues/Recommended-Insurance-Coverage-Criteria.pdf. [Accessibility verified December 27, 2019].
- Pérez-Panzano E, Gascón-Catalán A, Sousa-Domínguez R, et al. Reduction mammaplasty improves levels of anxiety, depression and body image satisfaction in patients with symptomatic macromastia in the short and long term. J Psychosom Obstet Gynaecol 2017;38:268-75. [Crossref] [PubMed]
- Emami SA, Sobhani R. Impact of reduction mammaplasty on sexuality in patients with macromastia and their partners. J Plast Reconstr Aesthet Surg 2016;69:1335-9. [Crossref] [PubMed]
- American Society of Plastic Surgeons. 2017 Plastic Surgery Statistics Report. Available online: https://www.plasticsurgery.org/documents/News/Statistics/2017/plastic-surgery-statistics-report-2017.pdf. [Accessibility verified December 27, 2019].
- Greco R, Noone B. Evidence-Based Medicine: Reduction Mammaplasty. Plast Reconstr Surg 2017;139:230e-9e. [Crossref] [PubMed]
- Bauermeister AJ, Gill K, Zuriarrain A, et al. Reduction mammaplasty with superomedial pedicle technique: A literature review and retrospective analysis of 938 consecutive breast reductions J Plast Reconstr Aesthet Surg 2019;72:410-8. [Crossref] [PubMed]
- Antony AK, Yegiyants SS, Danielson KK, et al. A matched cohort study of superomedial pedicle vertical scar breast reduction (100 breasts) and traditional inferior pedicle Wise-pattern reduction (100 breasts): an outcomes study over 3 years. Plast Reconstr Surg 2013;132:1068-76. [Crossref] [PubMed]
- Brownlee P, Chesire D, Crandall M, et al. Superomedial pedicle reduction mammaplasty: increased resection weight does not increase nipple necrosis. J Surg Res 2017;219:158-64. [Crossref] [PubMed]
- Makboul M, Abdelhamid M, Al-Attar G. Long Term Follow up and Patient Satisfaction after Reduction Mammoplasty: Superomedial versus Inferior Pedicle. World J Plast Surg 2017;6:82-7. [PubMed]
- Zehm S, Puelzl P, Wechselberger G, et al. Inferior pole length and long-term aesthetic outcome after superior and inferior pedicled reduction mammaplasty. Aesthetic Plast Surg 2012;36:1128-33. [Crossref] [PubMed]
- Robbins TH. A reduction mammaplasty with the areola-nipple based on an inferior dermal pedicle. Plast Reconstr Surg 1977;59:64-7. [Crossref] [PubMed]
- Erdogan B, Ayhan M, Deren O, et al. Importance of pedicle length in inferior pedicle technique and long-term outcome of areola-to-fold distance. Aesthetic Plast Surg 2002;26:436-43. [Crossref] [PubMed]
- Reus WF, Mathes SJ. Preservation of projection after reduction mammaplasty: long-term follow-up of the inferior pedicle technique. Plast Reconstr Surg 1988;82:644-52. [Crossref] [PubMed]
- Pitanguy I. Surgical treatment of breast hypertrophy. Br J Plast Surg 1967;20:78-85. [Crossref] [PubMed]
- Kemaloğlu CA, Özocak H. Comparative Outcomes of Inferior Pedicle and Superomedial Pedicle Technique With Wise Pattern Reduction in Gigantomastic Patients. Ann Plast Surg 2018;80:217-22. [Crossref] [PubMed]
- Hall-Findlay EJ. Vertical breast reduction with a medially-based pedicle. Aesthet Surg J 2002;22:185-94. [Crossref] [PubMed]
- Henderson PW, Chang MM, Taylor EM, et al. The "Superior Ledge": a Modification of the Standard Superomedial Pedicle Reduction Mammoplasty to Accentuate Nipple-Areola Complex Projection. Aesthetic Plast Surg 2016;40:733-8. [Crossref] [PubMed]
- Soussaline M. Mammoplasty. Inverted V technic. Analysis of 225 cases. Ann Chir Plast Esthet 1983;28:159-63. [PubMed]
- Chao JW, Taylor EM, Rohde CH. Reducing wound healing complications of Wise pattern breast reduction with the inverted "V" modification. J Plast Reconstr Aesthet Surg 2014;67:421-2. [Crossref] [PubMed]
- Hammond DC, Loffredo M. Breast reduction. Plast Reconstr Surg 2012;129:829e-39e. [Crossref] [PubMed]
- van Deventer PV. The blood supply to the nipple-areola complex of the human mammary gland. Aesthetic Plast Surg 2004;28:393-8. [Crossref] [PubMed]
- Michelle le Roux C, Kiil BJ, Pan WR, et al. Preserving the neurovascular supply in the Hall-Findlay superomedial pedicle breast reduction: an anatomical study. J Plast Reconstr Aesthet Surg 2010;63:655-62. [Crossref] [PubMed]
- Swanson E. Prospective outcome study of 106 cases of vertical mastopexy, augmentation/mastopexy, and breast reduction. J Plast Reconstr Aesthet Surg 2013;66:937-49. [Crossref] [PubMed]
- Spear ME, Nanney LB, Phillips S, et al. The impact of reduction mammaplasty on breast sensation: an analysis of multiple surgical techniques. Ann Plast Surg 2012;68:142-9. [Crossref] [PubMed]
- Mofid MM, Dellon AL, Elias JJ, et al. Quantitation of breast sensibility following reduction mammaplasty: a comparison of inferior and medial pedicle techniques. Plast Reconstr Surg 2002;109:2283-8. [Crossref] [PubMed]
- Manahan MA, Buretta KJ, Chang D, et al. An outcomes analysis of 2142 breast reduction procedures. Ann Plast Surg 2015;74:289-92. [Crossref] [PubMed]
- Wirthmann AE, Welsch L, Wellenbrock SV, et al. Reduction mammoplasty in adolescents and elderly: A ten year case series analyzing age related outcome with focus on safety and complications. J Plast Reconstr Aesthet Surg 2018;71:377-83. [Crossref] [PubMed]
- Landau AG, Hudson DA. Choosing the superomedial pedicle for reduction mammaplasty in gigantomastia. Plast Reconstr Surg 2008;121:735-9. [Crossref] [PubMed]
- Neaman KC, Armstrong SD, Mendonca SJ, et al. Vertical reduction mammaplasty utilizing the superomedial pedicle: is it really for everyone? Aesthet Surg J 2012;32:718-25. [Crossref] [PubMed]
- Rinker B. Lowering revision rates in medial pedicle breast reduction by the selective addition of "inverted-T" technique. Aesthetic Plast Surg 2013;37:341-8. [Crossref] [PubMed]
- Roehl K, Craig ES, Gómez V, et al. Breast reduction: safe in the morbidly obese? Plast Reconstr Surg 2008;122:370-8. [Crossref] [PubMed]
- Henry SL, Crawford JL, Puckett CL. Risk factors and complications in reduction mammaplasty: novel associations and preoperative assessment. Plast Reconstr Surg 2009;124:1040-6. [Crossref] [PubMed]
- Ogunleye AA, Leroux O, Morrison N, et al. Complications After Reduction Mammaplasty: A Comparison of Wise Pattern/Inferior Pedicle and Vertical Scar/Superomedial Pedicle. Ann Plast Surg 2017;79:13-6. [Crossref] [PubMed]
- Thoma A, Ignacy TA, Duku EK, et al. Randomized controlled trial comparing health-related quality of life in patients undergoing vertical scar versus inverted T-shaped reduction mammaplasty. Plast Reconstr Surg 2013;132:48e-60e. [Crossref] [PubMed]
- Fernandez S, Coady L, Cohen-Shohet R, et al. Comparative Outcomes and Quality Analysis of Inverted-T and Pure Vertical Scar Techniques in Superomedial Pedicle Reduction Mammaplasty. Ann Plast Surg 2016;76:S328-31. [Crossref] [PubMed]
- Young ZT, Close M, Herrera FA. National Surgical Quality Improvement Program Analysis of 9110 Reduction Mammaplasty Patients: Identifying Risk Factors Associated With Complications in Patients Older Than 60 Years. Ann Plast Surg 2019;82:S446-9. [Crossref] [PubMed]
- Baslaim MM, Al-Amoudi SA, Hafiz M, et al. The Safety, Cosmetic Outcome, and Patient Satisfaction after Inferior Pedicle Reduction Mammaplasty for Significant Macromastia. Plast Reconstr Surg Glob Open 2018;6:e1798. [Crossref] [PubMed]
- Hudson DA, Moodley S. Breast Reduction: Decreasing Complications and Improving Long-Term Aesthetic Results with Parenchymal Sutures. Plast Reconstr Surg Glob Open 2017;5:e1470. [Crossref] [PubMed]
- Simpson AM, Donato DP, Kwok AC, et al. Predictors of complications following breast reduction surgery: A National Surgical Quality Improvement Program study of 16,812 cases. J Plast Reconstr Aesthet Surg 2019;72:43-51. [Crossref] [PubMed]
Cite this article as: Grover K, Marano AA, Lin AJ, Peysakhovich A, Castillo W, Rohde CH. The modified Wise-pattern superomedial pedicle reduction mammoplasty for benign macromastia: a 9-year case series. Ann Breast Surg 2023;7:14.


