
The immediate-delayed deep inferior epigastric perforator (DIEP) flap: is it worth the extra step?—an expert’s opinion
Introduction
Breast cancer is the most common cancer in women worldwide (1). An increasing number of patients decide to undergo breast reconstruction after mastectomy (2). On local, regional, national and international level, a large variety exists among type and timing that are offered in breast reconstruction surgery. In general, autologous breast reconstructions are considered to provide a more natural and permanent outcome, resulting in higher patient-reported satisfaction rates when compared to implant-based reconstructions (3,4). Due to lower complication rates than other autologous flaps, the deep inferior epigastric perforator (DIEP) flap has become the golden standard for autologous breast reconstruction (5). The increasing number of DIEP flaps each year (6), requires a novel approach combining the most optimal oncological treatment on the one hand, while resulting in the most aesthetically pleasing breast(s) on the other hand. Moreover, in order to keep up with the increasing demand of DIEP flaps, efficient planning of the operation in support of reduction of surgical time is needed.
Immediate, immediate-delayed and delayed DIEP flap reconstruction
Following mastectomy, a DIEP flap reconstruction can be performed in an immediate, immediate-delayed (i.e., immediate tissue expander placement, followed by staged DIEP flap reconstruction) or delayed fashion. Several factors contribute to the decision-making process of the timing of the breast reconstruction, including medical considerations such as a history of breast surgery, comorbidities, patients’ anatomy or a possible indication for adjuvant radiotherapy (3,5,7,8). Moreover, patients’ preference, surgeons’ expertise and hospitals’ recourses are to be considered. For example, many hospitals do not have access to sufficient capacity to offer immediate breast reconstruction due to logistical challenges (9,10).
Given the varying risks and benefits of the different types of breast reconstructive options, the decision-making process can be highly complex and overwhelming for patients. This can lead to feelings of anxiety and/or distress in already uncertain times in which they are already confronted with the diagnosis of (increased risk at) breast cancer (11). Moreover, the Dutch guideline for breast cancer treatment advices a maximum period of six weeks between diagnosis and mastectomy (with or without breast reconstruction) (12), thereby putting a time constraint on the decision-making process. Previous literature showed that women who are struggling with their decision on what type of breast reconstruction to choose, experience additional emotional pressure due to this six week window (4). In order to buy time for decision-making process without delaying oncological treatment (i.e., the mastectomy, radiotherapy or adjuvant therapy) while preserving the skin envelop (13,14), immediate-delayed breast reconstruction might offer a solution to a possible lack of hospital capacity and/or perceived emotional pressure. In case the mastectomy was performed previously, a way to simulate a skin envelop, an extra procedure can be offered to pre-expand the breast skin that is left before performing the delayed breast reconstruction. DIEP flap reconstructions are cost-effective when considering health-related quality of life and patient satisfaction (15,16). However, comparative data on costs of pre-expansion of the breast before DIEP flap reconstruction is limited. Comparing immediate, immediate-delayed and delayed DIEP flap reconstruction, similar incidences of recipient site complications and flap re-explorations were observed (3).
The major advantage of pre-expansion of the breast is better cosmetic outcomes, in terms of better native shape of the breast, more sensate skin envelope and less scarring (5,7,8). This is important, because aesthetics play an important role in the quality of life and well-being of the patient and strongly influences the choice for additional reoperations (8). In addition, pre-expansion results in a shorter duration of reconstructive surgery for the autologous breasts.
However, there are also disadvantages to pre-expansion. First, an extra element of surgery during or after mastectomy is added, and the patient must live for a considerable amount of time with a tissue expander before definitive operation. This might lead to postponement of oncological therapy, may lead to longer hospitalization and increased risk of social or emotional difficulties due to complaints of the tissue expander or a prolonged time until completion of the treatment trajectory (5,8). Moreover, some patients experience the many out-clinic visits for expansion of the tissue expander as (emotionally) intensive. Last, the risk of early explantation of the tissue expander due to infection or erosion.
Clinical experience
Pre-operative consultation is crucial. Patients have a 30 minutes consultation at the plastic surgeon to show a standard PowerPoint with principles, examples of outcomes including a diverse range of photos, complications and treatment protocols. In case a patient is not convinced about her decision offering the option of pre-expansion after mastectomy might support patients in experiencing less pressure and stress during the decision-making process.
Indications for pre-expansion included all patients who underwent unilateral DIEP flap reconstruction between January 2013 and December 2019 or patients with the desire of a DIEP flap reconstruction who had their initial surgery (mastectomy) in another hospital, combined with patient-preference. The approach of pre-expansion consists of a skin sparing mastectomy followed by an immediate subpectoral placement of alloplastic material in form of a tissue expander and using them as spacers inside the breast skin envelop to avoid the skin to stick back to the thoracic wall after mastectomy has been performed. The tissue expander can be filled to enlarge the breast skin until the start of radiotherapy or adjuvant therapy, thereby not delaying oncological treatment. Once the oncological treatment is completed, the tissue expander can be filled until it is sufficient and substituted with the DIEP flap. During DIEP flap reconstruction, the tissue expander was removed and partial capsulectomy was performed. Premature explantation of the tissue expander due to infection or erosion occurred in seven patients (12.5%).
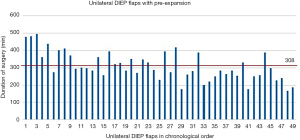
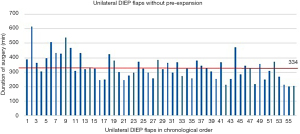
In our community hospital, the mean duration of surgery for unilateral DIEP flaps with pre-expanded breasts was 308 minutes (SD 81) and the mean duration of surgery for unilateral DIEP flap without pre-expanded breasts was 334 minutes (SD 85) (P=0.0126). Although not significant, it is clinically relevant. The duration of a DIEP flap in a pre-expanded breast is approximately 30 minutes shorter (Figures 1,2) with no more major complications, thereby creating opportunity to perform two unilateral DIEP flap reconstructions in one day.
Postoperative, patients with pre-expanded breasts were more satisfied with the aesthetics of the breast because of better native shape of the breast, more sensate skin envelope, no need for a (large) skin island, and less scarring. Hence a lower number of complementary surgeries were required to achieve satisfying aesthetic result.
Recommendation
According to previous literature and our clinical experience, the author’s opinion is that pre-expansion is worth the extra procedure. Pre-expansion of the breast leads to a shorter duration of reconstructive surgery with higher patients’ satisfaction rates and a comparable rate of complications. However, important factors to consider remain hospital capacity and costs. In future research, it would be valuable to include a costs-benefit analysis of both surgical modalities and to include patient-reported outcome (PRO) scores with a validated and breast cancer specific questionnaire such as BREAST-Q.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Tine Engberg Damsgaard and Jørn Bo Thomsen) for the series “Breast Reconstruction - The True Multidisciplinary Approach” published in Annals of Breast Surgery. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at: https://abs.amegroups.com/article/view/10.21037/abs-21-18/coif). The series “Breast Reconstruction - The True Multidisciplinary Approach” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Heer E, Harper A, Escandor N, et al. Global burden and trends in premenopausal and postmenopausal breast cancer: a population-based study. Lancet Glob Health 2020;8:e1027-37. [Crossref] [PubMed]
- Fertsch S, Munder B, Hagouan M, et al. Immediate-DElayed AutoLogous (IDEAL) breast reconstruction with the DIEP flap. Chirurgia (Bucur) 2017;112:387-93. [Crossref] [PubMed]
- Beugels J, Bod L, van Kuijk SMJ, et al. Complications following immediate compared to delayed deep inferior epigastric artery perforator flap breast reconstructions. Breast Cancer Res Treat 2018;169:349-57. [Crossref] [PubMed]
- Yueh JH, Slavin SA, Adesiyun T, et al. Patient satisfaction in postmastectomy breast reconstruction: A comparative evaluation of DIEP, TRAM, latissimus flap, and implant techniques. Plast Reconstr Surg 2010;125:1585-95. [Crossref] [PubMed]
- O’Connell RL, Di Micco R, Khabra K, et al. Comparison of immediate versus delayed DIEP flap reconstruction in women who require postmastectomy radiotherapy. Plast Reconstr Surg 2018;142:594-605. [Crossref] [PubMed]
- The Dutch Healthcare Authority. Declarations of microsurgical free flap reconstruction [Internet]. [cited 2021 Jan 24]. Available online: www.opendisdata.nl
- Kronowitz SJ. Delayed-immediate breast reconstruction: Technical and timing considerations. Plast Reconstr Surg 2010;125:463-74. [Crossref] [PubMed]
- Otte M, Nestle-Krämling C, Fertsch S, et al. Conservative mastectomies and Immediate-DElayed AutoLogous (IDEAL) breast reconstruction: The DIEP flap. Gland Surg 2016;5:24-31. [PubMed]
- Cima RR, Brown MJ, Hebl JR, et al. Use of lean and six sigma methodology to improve operating room efficiency in a high-volume tertiary-care academic medical center. J Am Coll Surg 2011;213:83-92. [Crossref] [PubMed]
- Sharma HR, Rozen WM, Mathur B, et al. 100 Steps of a DIEP Flap-A Prospective Comparative Cohort Series Demonstrating the Successful Implementation of Process Mapping in Microsurgery. Plast Reconstr Surg Glob Open 2019;7:e2016. [Crossref] [PubMed]
- Berlin NL, Tandon VJ, Hawley ST, et al. Feasibility and Efficacy of Decision Aids to Improve Decision Making for Postmastectomy Breast Reconstruction: A Systematic Review and Meta-analysis. Med Decis Making 2019;39:5-20. [Crossref] [PubMed]
- Netherlands Comprehensive Cancer Organisation (IKNL) [Internet]. [cited 2021 Jan 24]. Available online: https://www.iknl.nl
- DeBrock W, Pittelkow E. Abstract 75: Advantages Of The Delayed-Immediate Microsurgical Breast Reconstruction: Extending The Choice. Plast Reconstr Surg Glob Open 2020;8:48-9. [Crossref]
- McCarthy CM, Pusic AL, Disa JJ, et al. Unilateral postoperative chest wall radiotherapy in bilateral tissue expander/implant reconstruction patients: A prospective outcomes analysis. Plast Reconstr Surg 2005;116:1642-7. [Crossref] [PubMed]
- Matros E, Albornoz CR, Razdan SN, et al. Cost-effectiveness analysis of implants versus autologous perforator flaps using the BREAST-Q. Plast Reconstr Surg 2015;135:937-46. [Crossref] [PubMed]
- Khajuria A, Smith OJ, Prokopenko M, et al. Protocol for a systematic review and meta-analysis on the clinical outcomes and cost of deep inferior epigastric perforator (DIEP) flap versus implants for breast reconstruction. Syst Rev 2017;6:232. [Crossref] [PubMed]
Cite this article as: Jacobs JED, Bargon CA, Rakhorst HA. The immediate-delayed deep inferior epigastric perforator (DIEP) flap: is it worth the extra step?—an expert’s opinion. Ann Breast Surg 2022;6:1.

