
Bilateral male idiopathic granulomatous mastitis of the breast: a case report
Introduction
Granulomatous mastitis (GM) is a rare benign chronic inflammatory disease of the breast. The inflammatory response leading to granuloma formation is thought to be caused by infectious micro-organisms, sarcoidosis, foreign material, or autoimmune disease such as Granulomatosis with polyangiitis. All these conditions therefore must be excluded before a diagnosis of idiopathic granulomatous mastitis (IGM) can be made (1).
IGM, also known in the literature as idiopathic granulomatous lobular mastitis (IGLM) (1) usually affects parous women. The etiology of IGM remains unclear, however it has been reported to be associated with elevated hormonal levels, particularly prolactin; autoimmune diseases; diabetes; smoking; and lack of alpha 1-antitrypsin (2). More recently, Corynebacterium, a gram-positive bacillus endogenous to the skin, has been shown to be associated with IGM and that this organism may be the initial pathogenic insult responsible for generating an autoimmune response leading to granuloma formation. This infection demonstrates a distinct histologic pattern of cystic neutrophilic granulomatous mastitis (CNGM) (3,4).
As IGM affects mainly the mammary lobule, it is extremely rare in male patients. Gynecomastia is a possible predisposing factor for ductal or lobular-centric disease in males since terminal ductal lobular units do not normally develop in the male breast. We describe a rare case of biopsy-proven bilateral IGM in a male patient based on imaging and pathologic findings. There are a few reported cases of IGM in males (5-9). To the best of our knowledge, this is the first case of bilateral disease. We present the following case in accordance with CARE reporting checklist (available at https://abs.amegroups.com/article/view/10.21037/abs-20-155/rc).
Case presentation
A 46-year-old man presented to the Breast Diagnostic Clinic at Sunnybrook Hospital with a 6-month history of an unresolving left subareolar mass with purulent peri-areolar discharge for the past 4 weeks, and a new palpable subareolar mass on the right for the past 4 weeks. He had recently failed antibiotic treatment. He was known to have a long-standing history of a waxing and waning left-sided breast lump dating back to his twenties. His medical history is otherwise unremarkable except for prior appendectomy. His ethnic origin is identified as black. He is a non-smoker. On examination, there was visible swelling under the nipples, greater on the left than the right. The skin within the left peri-areolar region appeared inflamed with two sinus tracts seen at the 1:00 and 8:00 positions (shown in Figure 1).

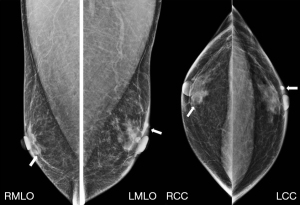
Bilateral mammography and ultrasound were performed. Left breast mammogram demonstrated an indistinct subareolar mass associated with diffuse peri-areolar skin thickening with a focal region of thickening favored to represent a draining sinus tract (shown in Figure 2). On ultrasound, this corresponded to an ill-defined irregular hypoechoic subareolar mass at the 4:00 location, measuring 3.8 cm × 2.0 cm × 1.6 cm with internal vascularity (shown in Figure 3A,3B). Sinus tracts with mobile content extending to the skin were confirmed on ultrasound (shown in Figure 3C). Multiple left axillary lymph nodes were asymmetrically prominent compared to the right but demonstrated cortical thickening within normal limits (shown in Figure 3D). Right breast mammogram demonstrated flame-shaped subareolar opacities in keeping with gynecomastia (shown in Figure 2). There was a mass within the medial subareolar region, corresponding on ultrasound to a lobulated, oval, heterogenous hypoechoic mass measuring 1.2 cm × 0.9 cm × 0.6 cm with cystic spaces (shown in Figure 3E,3F). There were no enlarged right axillary lymph nodes.

The bilateral subareolar breast masses were targeted for ultrasound-guided biopsy with a 14-guage needle. Left axillary node fine needle aspiration was also performed. On pathology, the left breast mass demonstrated benign breast parenchyma with mixed acute and chronic inflammation. Sampling from the left axillary lymph node was negative for malignancy and revealed a polymorphous population of lymphoid cells with germinal center fragments and tingible body macrophages consistent with a reactive process. Right breast mass sampling on pathology demonstrated benign breast tissue with necrotizing GM (shown in Figure 4A).
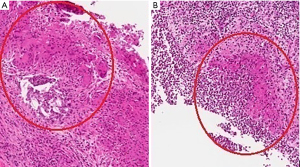
The patient returned 2 weeks later for re-biopsy of right breast GM for tissue culture in order to rule out important secondary causes of GM such as fungal, tuberculous and other bacterial infections. At this time, ultrasound of the right breast subareolar region demonstrated a complex collection in keeping with an abscess, the largest portion of the collection measured 3.4 cm × 0.8 cm × 1.7 cm. There was pus draining from the previous biopsy tract. Repeat ultrasound-guided core biopsy again revealed necrotizing granulomas (shown in Figure 4B). A histologic pattern of CNGM was not observed on any of the breast biopsy samples. Aspiration of the collection revealed many pus cells. No fungal elements, bacterial organisms or acid-fast bacilli were identified on special stains and on specimen cultures. The results demonstrated a sterile inflammatory process consistent with IGM, which was likely bilateral. The patient was treated with tapering doses of prednisone starting at 50 to 25 mg daily over 4 months. At the 3-month visit (shown in Figure 5), he was noted to have decreased swelling bilaterally and less drainage from the left peri-areolar sinus tract. He was not able to decrease his dosage below 25 mg of prednisone without reoccurring symptoms. Therefore, he was referred to Rheumatology to start methotrexate. After 6 months of methotrexate at 20 mg weekly and slow taper off prednisone, the patient had resolution of swelling bilaterally and peri-areolar drainage. He has had no further drainage or recurrence of symptoms two years after diagnosis. No adverse events were reported. The patient was pleased with the treatment and management of his symptoms.

All procedures performed in this case were in accordance with the ethical standards of the institutional research committee and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Discussion
The most common clinical finding on physical examination of patients with IGM is a solitary tender palpable lump (2). There have been a few reported cases of IGM in males, all of whom presented with a palpable unilateral breast lump (5-9). Our case is the first to present with bilateral disease. In women, IGM tends to have a prolonged course and is often complicated by ipsilateral or contralateral recurrence, poor healing, abscess formation, and fistulas, as demonstrated in our case. The clinical picture can present a challenge to clinicians as it can mimic inflammatory breast cancer or infection. Therefore, IGM remains a diagnosis of exclusion with breast carcinoma, chronic inflammatory conditions, infections and autoimmune diseases in the differential diagnosis.
On mammographic examination, IGM can demonstrate a density indistinguishable from gynecomastia, or reveal an asymmetry or irregular mass indistinguishable from breast carcinoma (2). Ultrasound typically reveals a hypoechoic heterogenous mass. Ultimately, core biopsy for histologic examination is required, which demonstrates granulomas with or without necrosis affecting mammary lobules, without any evidence of microorganisms. The definitive diagnosis of IGM can then be made by observing this histologic pattern and excluding all other possible causes of GM. While the diagnosis may be difficult, the clinician and radiologist suspect it when multiple sinus tracts are present on the breast.
Although the etiology of IGM is unclear, an autoimmune process is the most widely accepted theory (10). We did not find any evidence of immune dysfunction or systemic autoimmune disease in our patient. Unfortunately, an endocrinological work up or prolactin level was not performed, which may have been relevant. However, the patient demonstrated good response to methotrexate and steroid therapy. Prior to this, the disease course in our patient was chronic and progressive with no evidence of spontaneous remission, although long-term follow-up would be required to confirm remission and assess for any recurrence in our case. Before the 1980s, most patients with IGM were treated with wide surgical excision exclusively; however, conservative therapy with oral steroids, immunosuppressive or prolactin-lowering medication is being endorsed as a first-line treatment option, with surgery reserved for cases when pharmacological therapy has failed (2).
In summary, we presented the first case of bilateral IGM in a male patient. Although IGM is usually seen in parous women, it is important for clinicians to be aware of IGM and its presentation in males to be able to correlate typical clinical findings with imaging and biopsy in order to avoid extended antibiotic therapy. Our patient was found to have mild gynecomastia at presentation, which may have predisposed him to this rare disease. He was treated conservatively, initially using corticosteroids and demonstrated decreased swelling bilaterally and less drainage from the left peri-areolar sinus tract after 3 months, but ultimately achieved symptom resolution after 6 months of methotrexate with weaning off of corticosteroids. A better understanding of the pathogenesis and the mechanisms at the root of IGM may help establish a more targeted and non-invasive diagnostic and therapeutic protocol.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://abs.amegroups.com/article/view/10.21037/abs-20-155/rc
Peer Review File: Available at https://abs.amegroups.com/article/view/10.21037/abs-20-155/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://abs.amegroups.com/article/view/10.21037/abs-20-155/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional committee and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bakaris S, Yuksel M, Ciragil P, et al. Granulomatous mastitis including breast tuberculosis and idiopathic lobular granulomatous mastitis. Can J Surg 2006;49:427-30. [PubMed]
- Pluguez-Turull CW, Nanyes JE, Quintero CJ, et al. Idiopathic Granulomatous Mastitis: Manifestations at Multimodality Imaging and Pitfalls. Radiographics 2018;38:330-56. [Crossref] [PubMed]
- Taylor GB, Paviour SD, Musaad S, et al. A clinicopathological review of 34 cases of inflammatory breast disease showing an association between corynebacteria infection and granulomatous mastitis. Pathology 2003;35:109-19. [PubMed]
- Stary CM, Lee YS, Balfour J. Idiopathic granulomatous mastitis associated with corynebacterium sp. Infection. Hawaii Med J 2011;70:99-101. [PubMed]
- Reddy KM, Meyer CE, Nakdjevani A, et al. Idiopathic granulomatous mastitis in the male breast. Breast J 2005;11:73. [Crossref] [PubMed]
- Al Manasra AR, Al-Hurani MF. Granulomatous Mastitis: A Rare Cause of Male Breast Lump. Case Rep Oncol 2016;9:516-9. [Crossref] [PubMed]
- Joo L, Hyun Yeo S, Young Kwon S. Idiopathic Granulomatous Lobular Mastitis in a Male Breast: A Case Report. Iran J Radiol 2018;15:e55996. [Crossref]
- Farrokh D, Alamdaran A, Haddad AS, et al. Male granulomatous mastitis, a rarely encountered disorder. Breast J 2019;25:517-8. [Crossref] [PubMed]
- Sahin C, Agridag Ucpinar B. Idiopathic granulomatous mastitis in a male breast following intravesical Bacille Calmette-Guerin treatment. J Infect Public Health 2020;13:830-2. [Crossref] [PubMed]
- DeHertogh DA, Rossof AH, Harris AA, Economou SG. Prednisone management of granulomatous mastitis. N Engl J Med 1980;303:799-800. [Crossref] [PubMed]
Cite this article as: Madzima TR, Yuen V, Lu FI, Curpen B, Skarpathiotakis M. Bilateral male idiopathic granulomatous mastitis of the breast: a case report. Ann Breast Surg 2022;6:9.

