
Running breast cancer services in the National Health Service during COVID-19 pandemic, single center experience
Introduction
COVID-19 pandemic has severely affected health services safe practice all over the world. In United Kingdom (UK) and as part of the control measures a national lockdown was imposed early this year to control the infection rate, therefore the National Health Service (NHS) was to use its resources primarily to face the rising COVID-19 cases and other ongoing emergencies, limiting all non-urgent services to availability. Because of that, cancer services like breast cancer suffered significant interruption and delays. The accumulated effect of that was apparent after the lockdown measures were released, many institutions were and still facing a huge patient backlog that needs to be cleared to enable normal service resumption. To add another challenge, we are faced by a second pandemic wave threatening another lockdown.
Our institution at Sherwood Forest Hospitals Trust (SFH) managed to evolve and follow a successful breast cancer pathway that helped in keeping the necessary cancer services running, while protecting the staff and patients from acquiring the infection. After lifting the lockdown, we were in a good position to resuming normal service. Therefore, we think presenting our experience during the early months of the pandemic, and exchange ideas with other centres can help us all in facing the coming wave.
The Breast Service at SFH provides both symptomatic and screening services with a fully constituted multidisciplinary team, based at Kings Mill and Newark General Hospitals. Following COVID-19 outbreak, the screening service was suspended but the whole of the symptomatic service continued to be provided in line with national advice to change some of the pathways.
The new pathways developed at SFH aimed to minimise face to face contact while offering treatment to all patients with breast cancer diagnosis. The choice of treatments was based on molecular breast cancer subtypes and patient’s risks related to COVID-19 (1-3).
Until the time of writing this paper, there was little data on delivering breast cancer services in the NHS during the COVID-19 pandemic.
The aim of this study is to describe the performance data of delivering breast service at SFH during the COVID-19 pandemic.
Methods
Data for this study was collated retrospectively from the hospital information systems and including:
- General practitioner (GP) 2 weeks wait (2WW) referrals (suspected cancers);
- New cancer pathway;
- Telephone and face to face clinics;
- Theatre utilisation;
- Breast service backlog.
We compared the collected performance data during early lockdown period (March–April) to pre COVID-19 same period last year.
A prospective audit data for delayed 2WW patients was also collected using short questionnaire for consecutive cases, looking at the effect of delayed triple assessment.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethical approval was deemed unnecessary.
Results
Staffing
As a result of the COVID pandemic, some staffs were redeployed to Intensive Therapy Unit (ITU) and a small number became unavailable because of their need to shield, we were down by three doctors out of six and one breast care nurse (BCN) out of four. However, the remaining staffs were made adequate to maintain essential breast services. Regular team briefing was the cornerstone in keeping all the team informed and reorganized according to the national data and recommendations.
2WW referrals
An initial added telephone triaging step was introduced late in the study period for all patients referred under 2WW (Figure 1), although not perfect but it was shown in some studies to be a good alternative in the circumstances (4), and of these about 70% were converted to an urgent face to face consultation. The remaining 30% were given between 1–3-month appointments. Total number of patients triaged over March–April was 185, face to face consultations were 233, making a total of 418 clinic slots. Last year same period we used 564 slots, total number of diagnosed cancer over the study period was 35 compared to 43 last year (Table 1), the difference can be attributed to either missing cancers and/or the loss of the screening program detection which was 5.3 patients/month average in our institution (51 screen detected cancers in 2017, 77 in 2018, and 62 in 2019).

Table 1
| March–April 2019 | March–April 2020 | |
|---|---|---|
| Phone consultation | 0 | 185 |
| Face to face consultation | 564 | 233 |
| Total consultations | 564 | 418 |
| Detected cancers | 43 | 35 |
| Cancer follow up clinics | 105 | 95 |
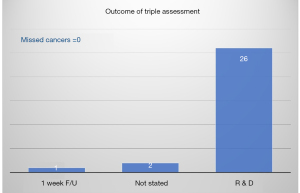
We audited our triage system as planned, 28 patients were delayed beyond the 2 weeks, 21/28 seen after more than one month. The audit outcome showed no cancers were missed due to the triaging step (Figure 2).
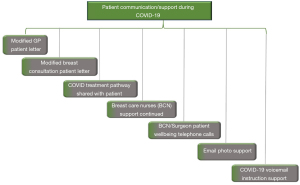
Clear communication protocol was introduced (Figure 3) to support patients during the pandemic specially delayed ones who were held in a patient treatment list (PTL) to avoid being lost to follow up.
Other clinics
Annual cancer follow-up clinics were changed to telephone consultations. Face to face reviews reserved for new cancer related complaint. Over the study period 95 patients were contacted, during same period in last year 105 patients were reviewed (Table 1).
All reconstruction clinics changed to teleclinics; patients informed of the service being on hold.
In addition to the planning of clinical capacity, the breast service was also required to estimate the personal protection equipment (PPE) requirements to deliver the planned face to face activity. For a 13-patient new clinic, for example, 273 pieces of basic PPE are required. Managing these resources was part of the overall changes.
Multi-disciplinary meetings (MDT)
Before COVID-19 we were running two meetings per week, those were combined in one meeting a week during the lockdown. Attendance was restricted to one member of each disciplinary with protective measures in place, others can join virtually.
Patients with operable cancer were prioritised for surgery based on cancer molecular biology and patient medical condition (5,6). Invasive triple negative, weakly oestrogen receptor (ER) positive, HER2 positive and poorly responsive to neoadjuvant chemotherapy patients prioritised over none invasive, ER positive and HER2 negative invasive ones. The latter group of patients had a marker clip inserted and commenced on neo-adjuvant endocrine treatment (NAET). While NAET is not a new treatment modality and being investigated (7), but this approach is gaining popularity in pandemic era (8).
Similarly, the provision of chemo and radiotherapy were modified in line with national guidance’s (9,10), where the risk for catching COVID-19 is riskier than the cancer itself (11).
Breast operative theatres
During the pandemic peak, all main theatres were changed into intensive care unit (ICU) beds. Surgical specialties were sharing 3 operating rooms, two for trauma and emergencies, and only one left for scheduled and elective procedures shared with urology, colorectal, upper GI surgery, and Ear, Nose, and Throat (ENT), dedicated specialty lists suspended. A new breast surgery pathway was devised (Figure 4) to continue operating under these circumstances while avoiding harm. Our prioritization system complied with published NHS specialty guidance (Figure 5) (12), to support ITU and free up sufficient number of inpatient beds. This would also meet the requirements of infection control by reducing footfall to the hospital and thereby protect patients and staff, especially high risk patients with poorer prognosis (12). Staff flexibility with working hours helped in using every available surgical slot, we operated on 26 out of 30 selected breast cancer patients in the first 6 weeks of the lockdown which enabled reducing the numbers in the waiting list. There were four on the day cancellation: 3 due to theatre staff shortage because of sickness and 1 due to unavailability of marker wire. No deaths or COVID related complications recorded.In line with national and trust guidelines, patients for surgery were screened for COVID with a microbiology swab and chest CT during the study period. The patients were also advised to self-isolate with their families for 14 days. Patients were admitted to the hospital the day before their surgery to allow COVID screening and undertake pre-operative assessment. Currently, guidance has changed, no CT chest is needed, patients to get their swab in a drive through booth within 72 hours of their operation and required to self-isolate after.
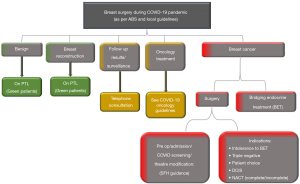
Face to face pre-operative consultation was not undertaken.
Theatre utilisation was reduced by about 50% compared to pre-COVID due to additional infection control measures such as PPE requirements and the absence of normal pre-operative assessment support.
Breast surgery backlog
The backlog of breast surgery cases in May 2020 is shown in comparison to other surgical specialities in the hospital is shown in (Table 2). Of the 67 breast cases, 30 were cancers the rest were benign or reconstruction procedures, the later cases were postponed following Association of Breast Surgeons recommendations (5). Pre COVID-19, the average waiting list for cancer surgery is about 20 cases and therefore as a result of the pandemic there was 10 extra cases, all of these cases were ER positive on NAET. Backlog cases are kept as red and green with detailed description and regular updates.
Table 2
| Specialty | Red | Amber | Green | Not recorded | Total |
|---|---|---|---|---|---|
| Breast surgery | 30 | – | 33 | 4 | 67 |
| Ear, nose, and throat (ENT) | 12 | 10 | 221 | 9 | 252 |
| General surgery | 9 | 55 | 391 | 54 | 509 |
| Maxillofacial surgery | 2 | 16 | 105 | – | 123 |
| Ophthalmology | – | 11 | 167 | 105 | 283 |
| Orthopaedics | 40 | 143 | 722 | 584 | 1,489 |
| Paediatric surgery | – | – | – | 7 | 7 |
| Urology | 45 | 154 | 228 | 33 | 460 |
| Vascular surgery | – | – | – | 33 | 33 |
| Grand total | 138 | 389 | 1,867 | 829 | 3,223 |
Discussion
Many studies were produced during the pandemic to demonstrate how to run services with strict infection control measures, some of these were related to breast cancer services (3,13,14), but none of them were based on NHS settings at the time of writing this paper. Therefore, their experience is not relevant to the NHS which follows a different local strict monitoring and supervision to ensure set cancer targets are met, for example Cancer Waiting Time (CWT) (15) like the 2WW between GP referral and patient being seen, also 62 days waiting time between referral and initiation of treatment, with many other set targets. Nevertheless, these studies confirm that breast cancer services can be safely maintained during the pandemic.
This study has demonstrated that essential breast cancer services can be delivered in the NHS during the COVID-19 pandemic. It has also shown that it can be done safely as there were no COVID related complications to either the patients or the staff. The 2WW target was met by the telephone consultation followed by urgent reviews, but the breach was inevitable in delayed reviews. Also NAET is considered as initiation of treatment but not meeting the 62 days wait for initiating definitive treatment.
During this period, there was adequate clinic and surgery capacity to provide service to the overall reduced workload due to reduction in GP referrals and on held screening services. New outpatient clinics pathways helped in preventing unnecessary contact during the pandemic peak helping patient and staff protection, the criteria avoided delaying cancer diagnosis as proved by our audit on the delayed triple assessment cases, the audit also showed patients understanding and appreciation of the difficult pandemic time, there was 2 out of 28 dissatisfied patients with the delay due to anxiety. As per national guidance, complex reconstructions and benign procedures were put on hold but we continued to do partial reconstructions with perforator flaps. For those patients with delayed cancer or reconstructive procedures we continued their follow up with three monthly telephone consultations to keep them well informed as well as assuring them they are still in our system and not forgotten.
From our experience we found that the operating time with PPE requirements has doubled compared to pre-COVID period, bearing that in mind help better planning of theatre slots, especially if we needed to go back to the shared lists system.
This study has also shown that it is important maintain undisturbed referral pathways to reduce the backlog that can eventually impact the service after lifting the lock down, this was apparent in some institutions, especially those who had to stop all elective services including cancers.
Threat of COVID-19 infection remains with expected bigger second wave. Therefore, strict infection control measures need to remain in place to protect patients and staff (16-18).
Based on this experience, the breast service at SFH continued with this current model for the duration of the pandemic and possibly continue with some of the positive learning in the long run.
Non urgent breast services such as breast screening had been paused during the crisis because the clinical gain is small with the large footfall and high risks of COVID cross infection. Nevertheless, it is useful to plan for re-opening these services, but a fixed date cannot be set until the safety conditions can be ensured. As to when that might be, it is difficult to predict, and the breast service recognises it may have to remain like this until a vaccine becomes available. Furthermore, given the lack of clear central guidance, the safety of re-opening each service is being left to the service after undertaking the appropriate risk assessment. Similarly, it is not always helpful to look at how other hospitals are managing a particular service because local circumstances vary and if this was the case then presumably, there would be unified guidance’s from the central government.
Whilst it was encouraging that the rate was falling initially because of the lockdown, hospital and care homes remain a concentrated pool for this infection. Therefore, based on the fact that up to 16% of staff is asymptomatic carriers beside admitted infected patients in the hospital makes it very dangerous for patients with non-urgent conditions to be bought in to the hospital. From a patient safety view, it is in the interest to stay out of hospital with the current infection rate unless their care is essential. Similarly, staff safety is of paramount and both central and Trust guidelines make this an important requirement.
The status of the cancer services that are currently running in our hospital is in a modified manner. Of course, the COVID crisis is still not over, and even with government’s partial relaxation of the lockdown, a partial lockdown will remain throughout the country and therefore, in the hospital itself. From an operational point of view, the difficulties in getting support from interdependencies are not expected to resolve very quickly. Staffs, who were shielding because of their high risk, are back to unrestricted duties with a ‘green area’ cannot be found for them easily, and hence the need to continue with the modified system.
Acknowledgments
Funding: None.
Footnote
Data Sharing Statement: Available at http://dx.doi.org/10.21037/abs-20-83
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/abs-20-83). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Xia Y, Jin R, Zhao J, et al. Risk of COVID-19 for patients with cancer. Lancet Oncol 2020;21:e180. [Crossref] [PubMed]
- Zhao L, Zhang L, Liu JW, et al. The treatment proposal for the patients with breast diseases in the central epidemic area of 2019 coronavirus disease. Zhonghua Wai Ke Za Zhi 2020;58:331-6. [PubMed]
- Liang W, Guan W, Chen R, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol 2020;21:335-7. [Crossref] [PubMed]
- Hollander JE, Carr BG. Virtually Perfect? Telemedicine for Covid-19. N Engl J Med 2020;382:1679-81. [Crossref] [PubMed]
- ABS. Association of Breast Surgery Statement, 27th April 2020 [Internet]. Available online: https:// associationofbreastsurgery.org.uk/for-members/covid-19-resources/
- Curigliano G, Cardoso MJ, Poortmans P, et al. Recommendations for Triage, Prioritization and Treatment of Breast Cancer PatientsDuring the COVID-19 Pandemic. the breast. Available online: https:// associationofbreastsurgery.org.uk/media/252022/covid-guidelines-european.pdf
- Spring LM, Gupta A, Reynolds KL, et al. Neoadjuvant Endocrine Therapy for Estrogen Receptor-Positive Breast Cancer: A Systematic Review and Meta-analysis. JAMA Oncol 2016;2:1477-86. [Crossref] [PubMed]
- Martí C, Sánchez-Méndez JI. Neoadjuvant endocrine therapy for luminal breast cancer treatment: a firstchoice alternative in times of crisis such as the COVID-19 pandemic. Ecancermedicalscience 2020;14:1027. [Crossref] [PubMed]
- RCR. Guidelines on radiation therapy for breast cancer during the COVID-19 pandemic [Internet]. Available online: https://www.rcr.ac.uk/college/coronavirus-covid-19-what-rcr-doing/clinical-information/coronavirus-covid-19-cancer
- Available online: https://www.nice.org.uk/guidance/ng161
- Lothian N. COVID-19 high and raised risk groups [Internet]. Available online: https://www.nhslothian.scot/ GetInvolved/Volunteering/Pages/COVID-19.aspx
- Coronavirus, Specialty guides [Internet]. [cited 2020 Jun 3]. Available online: https://www.england.nhs.uk/ coronavirus/secondary-care/other-resources/specialty-guides/#cancer
- Cortiula F, Pettke A, Bartoletti M, et al. Managing COVID-19 in the oncology clinic and avoiding the distraction effect. Ann Oncol 2020;31:553-5. [Crossref] [PubMed]
- Burki TK. Cancer guidelines during the COVID-19 pandemic. Lancet Oncol 2020;21:629-30. [Crossref] [PubMed]
- Delivering Cancer Waiting Timesa Good Practice Guide [Internet]. Available online: https://www.england.nhs.uk/ statistics/statistical-work-areas/cancer-waiting-times/
- Coronavirus (COVID-19) — Royal College of Surgeons [Internet]. [cited 2020 May 10]. Available online: https:// www.rcseng.ac.uk/coronavirus/
- PHE. Considerations for acute personal protective equipment (PPE) shortages [Internet]. Available online: https://associationofbreastsurgery.org.uk/for-members/ covid-19-resources/
- ABS. Guidance for ABS Members about Personal Protection Equipment (PPE) [Internet]. Available online: https://associationofbreastsurgery.org.uk/for-members/ covid-19-resources/
Cite this article as: Elamin G, Milburn N, Jahan A. Running breast cancer services in the National Health Service during COVID-19 pandemic, single center experience. Ann Breast Surg 2021;5:32.


