
The impact of tumour biology on the management of primary breast cancer in older women—based on a research programme in Nottingham
Background
The incidence of breast cancer increases with age (1). Due to improved survival outcomes and life expectancies, by 2040 around 40% of new breast cancer cases diagnosed per year globally, will be in patients aged ≥70 years (2). This will have a huge international impact both financially and in terms of service provision.
Despite this, most research in the field remains targeted at younger patients. Age-specific guidelines are not widely referred to and guidelines which do allude to the older woman as an individual are based solely on conventional factors, such as grade and size of tumour, nodal status and estrogen receptor (ER) status. The main treatment decisions in older (often defined using the age cut-off of 70 years in a number of studies) women with primary breast cancer are regarding (I) primary treatment and (II) adjuvant treatment.
Primary treatment
Current guidelines in the UK (3), Europe (4) and worldwide (5,6), advise surgery as the first-line treatment of primary operable breast cancer, irrespective of age. Historically, primary endocrine therapy (PET) has been used in older women unfit for surgery, or where the patient declines surgery. The International Society of Geriatric Oncology and European Society of Breast Cancer Specialists now advise that PET should only be offered for patients with ER-positive tumours with a limited life expectancy, despite optimisation of medical conditions (7). Despite this, figures for uptake of PET are reported between 12–40% (8-10).
Reasons for this are likely to be multifactorial and related to patient preferences, consideration of quality of life and physical fitness. One reason may be concerns over decline in health following surgery, however, there is limited evidence in the literature to support or deny the claim that functional status and independence decline after breast cancer surgery (11). Patients report good satisfaction and low treatment morbidity with PET (7). Furthermore, surgery and PET have similar survival outcomes for up to 5 years (10), thus PET appears to be an attractive treatment option in some patients. ER positivity is defined as staining of ≥1% of tumour nuclei in the sample tested (12). Although there is emerging data to suggest that samples which stain up to ≤10% ER-positive, behave in the same way as <1% ER-positive (13), the previous definition is still currently used. Overall, greater than 30% of patients with ER-positive primary breast cancer treated by surgery relapse despite endocrine therapy (14-16). In addition to this, initiation of PET can take weeks to months before any clinical benefit is seen and there is an unfortunate group of patients who exhibit no response following this.
Further problems arise in older women with primary breast cancer who have ER-negative tumours, of which there is little discussion in the current literature. There is little evidence to suggest that comorbidity itself is related to breast cancer subtype (17); one study has found a slightly lower proportion of ER-positive tumours among patients with diabetes (18).
Primary surgery is still recommended where possible. One alternative option is primary radiotherapy, which may present problems in terms of tolerability and side effects. Another option may be chemotherapy, however, it would be expected that if the patient could not tolerate surgical management, this would be the same, if not worse, for chemotherapy. Historically, some patients with ER-negative tumours received endocrine therapy regardless of receptor status (19) although this is no longer recommended (3).
Adjuvant treatment
No adjuvant treatment is risk-free and risks versus benefits of all potential treatments should be discussed with an older patient as part of the shared decision-making progress. Clearly, with use of multidrug therapy, risk of adverse events increases. The largest treatment dilemma in older women with regards to adjuvant treatment is whether or not they should receive adjuvant chemotherapy, especially in patients with ER-negative tumours where adjuvant endocrine therapy is not an option. Older patients tolerate chemotherapy poorly compared to their younger counterparts because of progressive reduction of organ function and comorbidities related to age (20).
A further dilemma is in the treatment of patients with human epidermal growth factor receptor 2 (HER2)-positive disease. Traditionally anti-HER2 therapies are offered in combination with chemotherapy. The National Surgical Adjuvant Study of Breast Cancer (N-SAS BC) 07 (RESPECT) trial is a phase 3 randomised trial in patients ≥70 years randomised to receive either trastuzumab or trastuzumab plus chemotherapy. The study has recruited 275 participants and the results are eagerly awaited (21). This could have significant implications for patients with HER2-positive disease if the benefit of trastuzumab alone is confirmed; meaning that they would only have to face the toxicity of a single treatment, which, in this case, has less side effects than chemotherapy.
Although generally, the side effects from adjuvant endocrine and radiotherapy are understood to be less detrimental than those of chemotherapy, they could be extremely significant in the group of patients who suffer from them. Studies have reported between 38–50% of patient discontinuation endocrine therapy within 5 years of surgery (22,23), largely thought to be related to intolerable side effects. Fatigue is the most common side effect following radiation therapy and affects up to 77% of patients (24).
Current understanding of breast cancer biology
Traditionally, we have understood breast cancer to consist of four main biological subtypes (Figure 1), with treatment plans dependent on subtype. Luminal A and B type tumours are more likely to respond to endocrine therapy; basal or triple negative breast cancer (TNBC) are most likely to benefit from chemotherapy and tumours with HER2 over-expression should be offered anti-HER2 therapy.

However, it is now recognised that breast cancer is a biologically heterogeneous complex of diseases, with a spectrum of many subtypes with distinct biological features (26). Therefore, treatment plans based on routinely measured biomarkers and our current understanding of disease subtypes may no longer be adequate.
The correlation between ER positivity and age is well documented; ER positivity increases with age with the highest proportion of patients with ER-positive tumours in the >65–70 years age group (27,28); >80% of older women tend to have ER-positive tumours (29), which is considered to be a less aggressive phenotype. This association is fundamental in the development of PET and adjuvant therapies in older women, however, we are now beginning to understand that there may be other biomarkers, not currently measured routinely in clinical practice, which may have importance in determining response to therapy (30).
Other favourable characteristics noted in older women with primary breast cancer are lower expression of HER2, lower frequency of p53 mutations and overexpression of B-cell lymphoma 2 (BCL-2) protein (31). Generally, breast cancers in older women appear to be more indolent and display less aggressive biological features. These features may help to guide treatment decision making where a patient may be considering surgery versus PET and when deliberating adjuvant therapies.
Some tools to help inform the prognosis and response to therapy, primarily in the adjuvant setting, do exist. The Nottingham Prognostic Index (NPI) (32), from our group, was the first tool of its kind to assess a combination of factors, including histological grade which reflects tumour biology, together with size of tumour and nodal status (time-dependent factors), to inform prognosis following surgery. Assessment that is more comprehensive, for example Adjuvant! Online (33), which uses more clinico-pathological features, has been developed, but recruitment of older women in their conception is lacking and the aims of these tools are not focused to the treatment dilemmas of the older population. Furthermore, these tools do not require unique tumour material to be assessed from an individual patient, so are not truly personalised to that patient (34).
Overview of Nottingham research programme
Breast cancer research in Nottingham has a longstanding international reputation since evolution of the Nottingham Grading System and NPI (32). We have experience in the study of breast cancer samples since our unit was established in 1973. The unit has since developed a unique research programme on primary breast cancer in older women.
The cohort
Over a 37-year period (1973–2010), 1,758 older (≥70 years) women with early operable (<5 cm, T0–2, N0–1, M0) primary breast cancer were managed in a dedicated facility in Nottingham. Clinical information was available from diagnosis of breast cancer until death or last documented follow-up and has been described previously (35,36). Histological data in terms of sample at diagnosis and surgical excision (SE) specimen (where applicable), is available. To the best of our knowledge, this is the largest database of this kind, in the literature.
Comparison between older and younger women
From the whole series, 813 patients underwent primary surgery and the remaining had non-operative or no treatment. It has been possible to construct 575 tissue microarrays (TMAs) using the SE samples and a panel of 25 biomarkers has been assessed in these SE TMAs (37). Cluster analysis identified six biological clusters of disease in older patients, four of which are consistent with standard clusters seen in younger women and one which was consistent with “normal-type” of breast tissue. The unique cluster, termed “low ER luminal” had high expression of luminal cytokeratins (CKs), mucin 1 and HER3 compared to the other conventional clusters and had different breast cancer specific survival (BCSS) compared to conventional clusters (Figure 2).

Primary treatment
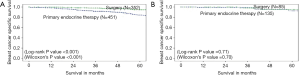
In a subset of 1,065 of the cohort, 449 had primary surgery and 616 PET. ER was measured by H-score and this was used as a continuous variable for analysis, rather than a standard cut-off. Patients with tumours with ER H-score of >250 (out of 300) (i.e., very ER rich) had equivalent BCSS regardless of treatment of primary surgery or PET (P=0.7) (Figure 3A), whereas in patients with H-score ≤250, surgery produced better BCSS (P<0.001) (Figure 3B) (35).
This suggests that within the group of patients with ER-positive disease based on standard definitions, there may be scope to further subdivide patients by the degree of ER-positivity.
In the overall cohort, 194 patients had ER-negative tumours, 77% of which were treated by primary surgery, 14.3% with PET (historic treatment), 5.6% with primary radiotherapy and supportive treatment only in 3.1% (38). Biological analysis did not demonstrate any correlation between measurement of PR, HER2 or Ki67 with BCSS, contrary to the findings in the patients with ER-positive tumours (35). However, compared to the patients with ER-positive tumours, patients with ER-negative tumours have higher rates of Ki67 expression, lower PR and higher HER2, consistent with more aggressive tumour biology. The majority of those with ER-negative tumours studied here, died of breast cancer in contrast to the outcome of patients with ER-positive tumours where the majority died of non-breast cancer causes.
After a comprehensive systematic literature review on the subject (39), a technique to successfully construct TMAs from core needle biopsy (CNB) samples was developed by us (40).
It has been possible to construct 693 TMAs from CNB samples from the overall cohort. A panel of 18 biomarkers has been measured in the majority of the CNB TMAs in patients who had ER-positive breast cancer (41). Examination of these specimens confirmed the presence of the low-ER luminal cluster and identified other biomarkers in addition to ER, which were independent predictors for BCSS, including PR, Ki67 and mucin 1 (41). It may be possible to determine which of these biomarkers help predict response to PET.
Adjuvant treatment
Findings suggestive of a diversification of biology (with differing clinical outcomes) according to age, have also been found in patients with HER-2 positive (42) and TNBC (43), providing evidence that consideration of the role of biology of breast cancer should be made during treatment decision making.
In a comparison study of 130 younger (<70 years) patients versus 43 older (≥70 years) patients identified as having HER2-postive tumours, there was no difference in BCSS, despite minimal use of chemotherapy in the older age group, compared to frequent use in the younger group (42). Furthermore, when compared to their younger counterparts, older women with HER2 overexpressing tumours were more likely to have low expression of Ki67 and high expression of BCL-2.
These results were replicated in patients with TNBC. A total of 127 older women with TNBC were compared to 342 younger women. The older patients with TNBC had lower expression of Ki67 and basal CK5/6, but higher expression of BCL-2 and luminal CK18. There was no significant difference in BCSS between younger and older women, despite minimal chemotherapy use in the older cohort.
These findings suggest that overall, older women in this cohort express a less aggressive phenotype of breast cancer, compared to their younger counterparts and provide evidence that consideration of the role of biology of breast cancer should be made during treatment decision making.
Future considerations
Fully understanding the biology of breast cancer in older women will impact every stage of the treatment pathway including primary and adjuvant treatment. For example, it may be possible to more accurately identify who will respond to endocrine therapy as primary treatment as an alternative to surgery, or which patients may not require adjuvant therapy. We hypothesise that there is a group of older women with breast cancer who will never die from their breast cancer due to competing comorbidities and being able to identify these patients at diagnosis would have a huge influence on their treatment.
A move is underway towards personalised cancer treatment, where tumour biology of an individual patient is examined to give unique predictive and prognostic information. This is extremely important in the setting of older women, who may have different treatment goals compared to their younger counterparts; their focus may be towards preservation of quality of life rather than curative treatment. There are currently a number of existing predictive and prognostic tools available for use in breast cancer, however, the evidence base for the use of these tools specifically in the older population is weak (34). Furthermore, these tools have mainly been licensed for use in the adjuvant setting following surgery. In the future, we expect the development of a tool to analyse an extensive panel of biomarkers for an individual patient with primary breast cancer, based on their CNB specimen. This would generate patient-specific survival outcomes based on their individual tumour biology, which would allow them to make personalised treatment decisions.
Some areas of medicine, for example, orthopaedic surgery, routinely utilise geriatric assessment (GA) to identify patients who may benefit from more detailed interventions. GA generally consists of a few major components including: medical assessment of current diagnoses, medications and nutritional status; assessment of physical function, psychological evaluation of mentality and mood; social and environmental assessments (44). The concept of GA in oncology is recommended (45), however, full GA can be time-consuming and may not be useful in all cases. Some studies have opted for use of a frailty screening assessment to decide who should receive full GA, but which tool best serves this purpose remains debatable (46,47).
A combination of detailed biological assessment, alongside some form of GA, would truly personalise breast cancer treatment for older women. Given our expanding older population as described, the health and economic implications of this on a worldwide scale can no longer be ignored.
Acknowledgments
Funding: No funding or sponsorship was received for the publication of this article. This article was written as part of RM Parks’ PhD, supported by a Fellowship funded by Nottingham Hospitals Charity, UK and an Honorary Fellowship from the Royal College of Surgeons of England. The overall project is supported by a grant funding by Breast Cancer Research Trust, UK.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/abs-20-130). KLC serves as an unpaid editorial board member of Annals of Breast Surgery from Aug 2020 to Jul 2022. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Elements related to the study of participant data was approved by the Nottingham Research and Development committee. The title of the application was “Development of a molecular genetic classification of breast cancer”, project registration number: 03HI01, ethics committee number: C1080301.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- UK CR. Breast cancer incidence (invasive) statistics. Available online: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/breast-cancer/incidence-invasive#heading-Zero [Accessed: 6th April 2020]. 2020.
- World Health Organisation. International Agency for Research on Cancer. Available online: https://www.iarc.fr [Accessed: 24th June 2019]. 2019.
- National Guideline Alliance (UK). Early and locally advanced breast cancer: diagnosis and management. London: National Institute for Health and Care Excellence (UK); 2018 Jul. NICE Guideline, No. 101.
- Senkus E, Kyriakides S, Ohno S, et al. Primary breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2015;26:v8-30. [Crossref] [PubMed]
- National Comprehensive Cancer Network. Breast Cancer: Early Stage. Version 1. 2016. Available online: https://www.nccn.org/patients/
- Kaufmann M, Morrow M, von Minckwitz G, et al. Locoregional treatment of primary breast cancer. Cancer 2010;116:1184-91. [Crossref] [PubMed]
- Biganzoli L, Wildiers H, Oakman C, et al. Management of elderly patients with breast cancer: updated recommendations of the International Society of Geriatric Oncology (SIOG) and European Society of Breast Cancer Specialists (EUSOMA). Lancet Oncol 2012;13:e148-60. [Crossref] [PubMed]
- Morgan J, Richards P, Ward S, et al. Case-mix analysis and variation in rates of non-surgical treatment of older women with operable breast cancer. Br J Surg 2015;102:1056-63. [Crossref] [PubMed]
- Morgan J, Wyld L, Collins KA, et al. Surgery versus primary endocrine therapy for operable primary breast cancer in elderly women (70 years plus). Cochrane Database Syst Rev 2014;(5):CD004272 [Crossref] [PubMed]
- Hind D, Wyld L, Beverley CB, et al. Surgery versus primary endocrine therapy for operable primary breast cancer in elderly women (70 years plus). Cochrane Database Syst Rev 2006;CD004272 [Crossref] [PubMed]
- Parks R. Impact of breast cancer surgery on functional status and independence. J Geriatr Oncol 2019;10:S1. [Crossref]
- Hammond ME, Hayes DF, Dowsett M, et al. American Society of Clinical Oncology/College of American Pathologists Guideline Recommendations for Immunohistochemical Testing of Estrogen and Progesterone Receptors in Breast Cancer. Arch Pathol Lab Med 2010;134:e48-72. [Crossref] [PubMed]
- Fujii T, Kogawa T, Dong W, et al. Revisiting the definition of estrogen receptor positivity in HER2-negative primary breast cancer. Ann Oncol 2017;28:2420-8. [Crossref] [PubMed]
- Haque MM, Desai KV. Pathways to Endocrine Therapy Resistance in Breast Cancer. Front Endocrinol (Lausanne) 2019;10:573. [Crossref] [PubMed]
- Piggott L, Silva A, Robinson T, et al. Acquired Resistance of ER-Positive Breast Cancer to Endocrine Treatment Confers an Adaptive Sensitivity to TRAIL through Posttranslational Downregulation of c-FLIP. Clin Cancer Res 2018;24:2452. [Crossref] [PubMed]
- Szostakowska M, Trębińska-Stryjewska A, Grzybowska EA, et al. Resistance to endocrine therapy in breast cancer: molecular mechanisms and future goals. Breast Cancer Res Treat 2019;173:489-97. [Crossref] [PubMed]
- Søgaard M, Thomsen RW, Bossen KS, et al. The impact of comorbidity on cancer survival: a review. Clin Epidemiol 2013;5:3-29. [Crossref] [PubMed]
- Chlebowski RT, McTiernan A, Wactawski-Wende J, et al. Diabetes, metformin, and breast cancer in postmenopausal women. J Clin Oncol 2012;30:2844-52. [Crossref] [PubMed]
- Syed BM, Morgan DAL, Setty T, et al. Oestrogen receptor negative early operable primary breast cancer in older women—Biological characteristics and long-term clinical outcome. PLoS One 2017;12:e0188528 [Crossref] [PubMed]
- Rossi A, Colantuoni G, Maione P, et al. Chemotherapy of Breast Cancer in the Elderly. Curr Med Chem 2005;12:297-310. [Crossref] [PubMed]
- U.S. National Library of Medicine. National Surgery Adjuvant Study of Breast Cancer (N-SAS BC) 07 (RESPECT). Available online: https://clinicaltrials.gov/ct2/show/study/NCT01104935 [Accessed 5th April 2020]. ClinicalTrials.gov 2019.
- Hagen KB, Aas T, Kvaløy JT, et al. Adherence to adjuvant endocrine therapy in postmenopausal breast cancer patients: A 5-year prospective study. Breast 2019;44:52-8. Erratum in: Breast 2019 Jun;45:118. doi: 10.1016/j.breast.2019.03.007. Epub 2019 Apr 5. [Crossref] [PubMed]
- Robinson B, Dijkstra B, Davey V, et al. Adherence to Adjuvant Endocrine Therapy in Christchurch Women with Early Breast Cancer. Clin Oncol (R Coll Radiol) 2018;30:e9-e15. [Crossref] [PubMed]
- Lipsett A, Barrett S, Haruna F, et al. The impact of exercise during adjuvant radiotherapy for breast cancer on fatigue and quality of life: A systematic review and meta-analysis. Breast 2017;32:144-55. [Crossref] [PubMed]
- Dai X, Li T, Bai Z, et al. Breast cancer intrinsic subtype classification, clinical use and future trends. Am J Cancer Res 2015;5:2929-43. [PubMed]
- Yersal O, Barutca S. Biological subtypes of breast cancer: Prognostic and therapeutic implications. World J Clin Oncol 2014;5:412-24. [Crossref] [PubMed]
- Kerlikowske K, Gard CC, Tice JA, et al. Risk Factors That Increase Risk of Estrogen Receptor-Positive and -Negative Breast Cancer. J Natl Cancer Inst 2016;109:djw276 [Crossref] [PubMed]
- Rhodes A, Jasani B, Balaton AJ, et al. Frequency of oestrogen and progesterone receptor positivity by immunohistochemical analysis in 7016 breast carcinomas: correlation with patient age, assay sensitivity, threshold value, and mammographic screening. J Clin Pathol 2000;53:688-96. [Crossref] [PubMed]
- Diab SG, Elledge RM, Clark GM. Tumor characteristics and clinical outcome of elderly women with breast cancer. J Natl Cancer Inst 2000;92:550-6. [Crossref] [PubMed]
- Parks RM, Cheung KL. Clinical relevance of biomarkers in oestrogen receptor positive breast cancer. In: Chen GG, Tong MCF, van Hasselt CA. editors. Estrogen Receptors: Structure, Functions and Clinical Aspects. 1st edition. New York, USA: Nova Science Publishers, 2020:53-91.
- Dimitrakopoulos FI, Kottorou A, Antonacopoulou AG, et al. Early-Stage Breast Cancer in the Elderly: Confronting an Old Clinical Problem. J Breast Cancer 2015;18:207-17. [Crossref] [PubMed]
- Haybittle JL, Blamey RW, Elston CW, et al. A prognostic index in primary breast cancer. Br J Cancer 1982;45:361-6. [Crossref] [PubMed]
- de Glas NA, van de Water W, Engelhardt EG, et al. Validity of Adjuvant! Online program in older patients with breast cancer: a population-based study. Lancet Oncol 2014;15:722-9. [Crossref] [PubMed]
- Gordon-Craig S, Parks RM, Cheung KL. The Potential Use of Tumour-Based Prognostic and Predictive Tools in Older Women with Primary Breast Cancer: A Narrative Review. Oncol Ther 2020;8:231-50. [Crossref] [PubMed]
- Syed BM, Al-Khyatt W, Johnston SJ, et al. Long-term clinical outcome of oestrogen receptor-positive operable primary breast cancer in older women: a large series from a single centre. Br J Cancer 2011;104:1393-400. [Crossref] [PubMed]
- Syed BM, Johnston SJ, Wong DWM, et al. Long-term (37 years) clinical outcome of older women with early operable primary breast cancer managed in a dedicated clinic. Ann Oncol 2012;23:1465-71. [Crossref] [PubMed]
- Syed BM, Green AR, Paish EC, et al. Biology of primary breast cancer in older women treated by surgery: with correlation with long-term clinical outcome and comparison with their younger counterparts. Br J Cancer 2013;108:1042-51. [Crossref] [PubMed]
- Syed BM, Morgan D, Setty T, et al. Oestrogen receptor negative early operable primary breast cancer in older women-Biological characteristics and long-term clinical outcome. PloS one 2017;12:e0188528 [Crossref] [PubMed]
- Albanghali M, Green A, Rakha E, et al. Construction of tissue microarrays from core needle biopsies - a systematic literature review. Histopathology 2016;68:323-32. [Crossref] [PubMed]
- Albanghali M. Biology and clinical outcomes of early primary breast cancer in older women - a study based on core needle biopsy. PhD Thesis. University of Nottingham, November, 2016.
- Parks RM, Albanghali M, Syed BM, et al. Biology of Oestrogen-Receptor Positive Primary Breast Cancer in Older Women with Utilisation of Core Needle Biopsy Samples and Correlation with Clinical Outcome. Cancers (Basel) 2020;12:2067. [Crossref] [PubMed]
- Syed BM, Green AR, Ellis IO, et al. Human epidermal growth receptor-2 overexpressing early operable primary breast cancers in older (≥70 years) women: biology and clinical outcome in comparison with younger (<70 years) patients. Ann Oncol 2014;25:837-42. [Crossref] [PubMed]
- Syed BM, Green AR, Nolan CC, et al. Biological characteristics and clinical outcome of triple negative primary breast cancer in older women - comparison with their younger counterparts. PLoS One 2014;9:e100573 [Crossref] [PubMed]
- Parks RM, Lakshmanan R, Winterbottom L, et al. Comprehensive geriatric assessment for older women with early breast cancer - a systematic review of literature. World J Surg Oncol 2012;10:88. [Crossref] [PubMed]
- Wildiers H, Heeren P, Puts M, et al. International Society of Geriatric Oncology consensus on geriatric assessment in older patients with cancer. J Clin Oncol 2014;32:2595-603. [Crossref] [PubMed]
- Biganzoli L, Mislang AR, Di Donato S, et al. Screening for Frailty in Older Patients With Early-Stage Solid Tumors: A Prospective Longitudinal Evaluation of Three Different Geriatric Tools. J Gerontol A Biol Sci Med Sci 2017;72:922-8. [Crossref] [PubMed]
- Valentini A, Federici M, Cianfarani MA, et al. Frailty and nutritional status in older people: the Mini Nutritional Assessment as a screening tool for the identification of frail subjects. Clin Interv Aging 2018;13:1237-44. [Crossref] [PubMed]
Cite this article as: Parks RM, Green AR, Cheung KL. The impact of tumour biology on the management of primary breast cancer in older women—based on a research programme in Nottingham. Ann Breast Surg 2021;5:5.

