
A case of locoregional recurrence of breast cancer in the interpectoral lymph nodes—an unusual location
Introduction
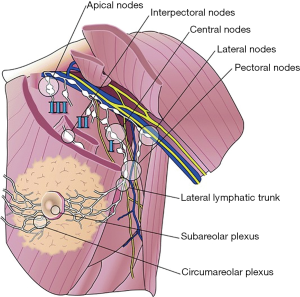
The emigration of breast cancer—metastasis to the axilla normally follows a regular pattern from level I to level II and last level III, and the percentage of skipping metastases is low (1). Level I lymph nodes include lymph nodes lateral to the pectoralis minor muscle, level II lymph nodes are located posterior to the pectoralis minor muscle, and lymph nodes in level III consist of lymph nodes medial to the pectoralis minor muscle (Figure 1). Studies have shown involvement of interpectoral lymph nodes (IPN) in up to 14% of case of breast cancer at the time of operation (3,4). Little is known about the incidence of recurrence at this site, but one retrospective study showed 0.1% of recurrence in the IPN (5). The IPN are located between the pectoralis major and minor muscles in the interpectoral fascia, and were first described by Grossman and later by Rotter (Figure 1). The IPN are also known as “Rotter’s nodes” (6,7).
Case presentation
A 54-year-old women underwent mastectomy in 2012 due to a 19 mm invasive ductal carcinoma (IDC) located in the upper half of the left breast with micrometastasis to the axilla. According to guidelines axillary lymph node dissection was not performed. The patient had adjuvant treatment including chemotherapy, anti-estrogen treatment, and Herceptin treatment. In 2014, the patient had reconstruction of the breast with breast implant, nipple-areola complex reconstruction, and reduction of the contralateral breast. Due to unsatisfying symmetry at the final clinical assessment, the patient was offered a re-reduction of the right breast. As a standard procedure, a mammography is performed preoperatively, and a malignant mass was discovered superior to the implant in the left breast. Ultrasound and positron emission tomography-computed tomography (PET-CT) verified 4 malignant tumors located interpectoral also known as Rotter’s space, and fine needle aspiration revealed IDC. The biopsies, performed twice, were not able to verify lymphatic tissue. It was not possible to palpate defined tumor, only increased tissue filling. Surgically removal of the tumors was performed in cooperation with a plastic surgeon leaving the breast implant in situ. Five tumors were removed. Subsequently histological examination confirmed lymph node metastasis from IDC in all 5 tumors. Adjuvant radiotherapy of the breast is planned postoperatively.
Discussion
This is a case of locoregional recurrence located in the IPN found on a routine mammography prior to reduction of the contralateral breast. At the time of diagnosis there was not palpable tumors in the area. In a retrospective study, where 0.1% had recurrence in the IPN, lesions were not demonstrated on a mammography, but on the contrary to our case, all patients had palpable masses in the region (5). It is therefore important to notice that neither physical examination nor mammography can stand alone in the diagnosis of recurrence in the IPN. In this case, ultrasound was able to visualize and confirm the location of the recurrence, but the sensitivity of ultrasound detection of IPN involvement has earlier been reported to 33%, giving a false negative rate at 67% (8). It is earlier hypothesized that patients with tumors located in the upper half of the breast have a higher risk of developing regional recurrences in the IPN, but this hypothesis was not supported by a retrospective study of recurrence in the IPN (5). This case also raises the question whether IPN can be sentinel nodes. When axillary dissection of level I and II was considered gold standard of treatment of early-stage, ultrasound node-negative cancer, it was proposed in one study that the IPN should be included in the axillary dissection (9). Now that sentinel node biopsy is the preferred procedure in patients with breast cancer without axillary metastases detectable by axillary ultrasound, it is important to acknowledge the possibility of IPN being sentinel nodes. Researchers found that the interpectoral nodes drain to level II and apical lymph nodes of the axilla, and therefore concluded that IPN could act as sentinel nodes without involvement of the level I lymph nodes (10). The most interesting cases are patient with IPN metastases without axillary metastases. Though the quantity of such cases is found low from 0.3% to 7% (3,4,11), it could contribute to the risk of axillary recurrence. Even though this localization of recurrence is rare, it is important to bear in mind because of difficult clinical presentation, and because it has shown not to be visible on mammography. Little is known about the incidence of recurrence at this anatomical location and not much research has been done. Further studies should be carried out as this site represents a potential site of locoregional recurrence.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/abs.2019.03.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Veronesi U, Luini A, Galimberti V, et al. Extent of Metastatic Axillary Involvement in 1446 Cases of Breast Cancer. Eur J Surg Oncol 1990;16:127-33. [PubMed]
- Jatoi I, Rody A. Management of Breast Diseases. Springer 2016:247-71.
- Cody HS, Egeli RA, Urban JA. Rotter's Node Metastases. Ann Surg 1984;199:266-70. [Crossref] [PubMed]
- Dixon JM, Dobie V, Chetty U. The Importance of Interpectoral Nodes in Breast Cancer. Eur J Cancer 1993;29A:334-6. [Crossref] [PubMed]
- Komenaka IK, Bauer VP, Schnabel FR, et al. Interpectoral Nodes as the Initial Site of Recurrence in Breast Cancer. Arch Surg 2004;139:175-8. [Crossref] [PubMed]
- Grossmann F. Ueber die Axilaren Lymphdrusen: Ianugural Dissertation. Berlin, Germany: C Vogt, 1986.
- Rotter J. Topagraphie des Mamma-Carcinom. Arch fur Klinische Chirurgie 1899;58:346-56.
- Oran I, Memiş A, Ustün EE. Ultrasonographic detection of interpectoral (Rotter's) node involvement in breast cancer. J Clin Ultrasound 1996;24:519-22. [Crossref] [PubMed]
- Chandawarkar RY, Shinde SR. Interpectoral nodes in carcinoma of the breast: requiem or resurrection. J Surg Oncol 1996;62:158-61. [Crossref] [PubMed]
- Bale A, Gardner B, Shende M, et al. Can interpectoral nodes be sentinel nodes? Am J Surg 1999;178:360-1. [Crossref] [PubMed]
- Kay S. Evaluation of Rotter's Lymph Nodes in Radical Mastectomy Specimens as a Guide to Prognosis. Cancer 1965;18:1441-4. [Crossref] [PubMed]
Cite this article as: Hansen SM, Hoyer U. A case of locoregional recurrence of breast cancer in the interpectoral lymph nodes—an unusual location. Ann Breast Surg 2019;3:6.

