Prophylactic mastectomy can save patients up to $50,000 compared to lifelong screening in BRCA 1 and BRCA 2 patients
Introduction
Healthcare continues to advance in both treatment and screening for breast cancer, especially in high-risk women. At the same time, both patient and healthcare funds are limited. As physicians, it is imperative that we monitor the value of the services we provide ensuring both affordable and effective care. Patients with BRCA1 or BRCA2 mutations are at dramatically higher risk for developing breast cancer compared to the general population with a lifetime risk up to 87% by age 70 (1). There are several options to care for a woman with a BRCA mutation carrier. Current recommendations include the option of increased screening, chemoprevention, and risk-reducing surgeries. The decision is a personal one with women often initially choosing screening and desire risk-reducing surgery thereafter (2).
The current National Comprehensive Cancer Network (NCCN) screening recommendations for BRCA mutation carriers include biannual clinical breast exam beginning at age 25 along with an annual MRI then adding annual screening mammography, beginning at age 30 (3). The use of both mammography and MRI in high risk patients is to identify abnormalities earlier with higher sensitivity and specificity. Screening trials in BRCA patients have shown 89–100% of breast cancers were detected with the combination of MRI and mammography and only 33–50% with mammography alone. However, with the added sensitivity comes a higher false positive rate. The false positives lead to additional imaging and often biopsy (4,5). However, several studies have shown this strategy is cost-effective as it detects cancer earlier rather than at a more advanced stage. Due to the earlier detection of breast cancer with MRI in high risk patients, the overall benefit outweighs the additional screening cost and higher risk of false positives (6,7).
For high-risk women who choose risk-reducing surgery, a bilateral mastectomy with the option of reconstruction is offered. Compared to screening, surgery offers the benefit of cancer risk reduction. The PROSE study demonstrated a 90% breast cancer risk reduction in BRCA1 or BRCA2 carriers who underwent bilateral mastectomy with intact ovaries and a 95% reduction in breast cancer risk for women who undergo concomitant oophorectomy (8).
Our goal is to compare the expense of lifelong screening versus prophylactic mastectomy with reconstruction for BRCA 1 and 2 patients to evaluate potential cost-savings from a patient perspective. Although the cost of early detection and cancer prevention has been confirmed, to our knowledge we are the first to compare the cost of screening versus surgery from both the patient and healthcare perspectives.
Methods
A projected cost analysis was performed to estimate the cost of lifelong screening versus bilateral mastectomy with deep inferior epigastric perforator (DIEP) flap reconstruction in female patients within our health system between the ages of 25–75 with a BRCA mutation. This study was IRB approved. NCCN guidelines recommend surveillance from age 25–75 so these ages were included for the lifespan (3). The CPT codes were identified for an established visit, digital mammography with computer aided detection (CAD), 3D rendering, MRI with CAD, and the radiology interpretation fee. The total screening cost was estimated by adding these costs as calculated for the patient as well as for the insurance company. The total cost for surgery was the combined costs of the operating room time, the surgeon, the plastic surgeon, the hospital, and anesthesia fees. In order to analyze a final cost we utilized a combination of a price hotline available at our institution as well as the hospital-generated bills from 10 de-identified patients which were averaged to confirm the amount that the patient and insurance company actually pay. Finally, the high-risk screening costs were calculated to show the difference between upfront surgery versus a lifetime of screening. The patient out of pocket payments were estimated based on a hypothetical insurance plan with a deductible of $1,000, an 80/20 copay, and a $5,000 annual out of pocket maximum. For the surveillance group, we estimated the cost of annual screening mammogram and annual contrast enhanced MRI. We included the cost of one additional office visit per year for a total of 45 years (ages 30–75). The CPT codes used for mammography included CAD as well as 3D rendering which is more costly than screening mammography alone but is the recommended modality by the American College of Radiology for high risk patients (9).
Results
The cost of high-risk breast screening is summarized in Table 1. The amount attributed to the patient is dependent on her insurance plan. The total out of pocket charge will be the total charge minus the insurance plan coverage. The mammogram charge is included in most insurance plans, so it is calculated at $0 for the patients and $116 for the insurance company.
Table 1
| Description of code | CPT code | Total charge |
|---|---|---|
| Level 3 established patient visit | 99213 | $146 |
| Mammogram | 77057 | $116, $0 to the patient |
| Radiology fee Medicare | $171 | |
| MRI with CAD | 77059, 0159T | $2,294 |
| Total charge | $2,611 |
CAD, computer aided detection.
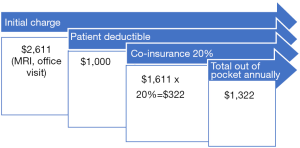
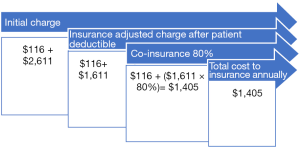
In our hypothetical insurance plan, the patient pays an initial $1,000 deductible. Of the remaining bill, 20% is charged to the patient. The 20% ($322) is added to the deductible ($1,000) for a total annual out of pocket for the patient of $1,322 (Figure 1). The insurance company pays the remaining $1,405 [($1,611×0.8) + $116] (Figure 2). This is the annual payment assuming no biopsies or additional imaging is required.
When a patient chooses risk-reducing bilateral mastectomy as the initial option following identification of a BRCA mutation, the patient will pay her out-of-pocket maximum as a one-time cost. We used an estimate of $5,000 as a hypothetical out of pocket maximum, but this may vary based on a specific insurance plan. The prophylactic surgery charges, costs, and re-imbursement are listed in Table 2 below.
Table 2
| Description of code | Initial charge | Average reimbursement |
|---|---|---|
| Bilateral mastectomy with DIEP flap reconstruction: OR specific costs | $140,915 | $65,744 |
| Additional hospital days: average 3 | $38,164 | $17,937 |
| Plastic surgeon charge | $20,000 | $9,400 |
| Anesthesia charge: 8 hours | $3,515 | $1,652 |
| Total costs: one time | $202,594 | $94,733 |
DIEP, deep inferior epigastric perforator.
Of the $94,733, the patient will pay the max out of pocket, an estimated $5,000 and the remainder would be paid by the insurance company—$89,733.
As the patient is not charged for a screening mammogram, her costs are the same annually for surveillance. The insurance company pays $1,289 annually for the first 5 years then $1,405 annually for the next 46 years for screening for ages 30–75. The cumulative cost for the patient, insurance, and healthcare system is shown below in Table 3.
Table 3
| Year | Patient cost | Insurance cost | Patient + insurance |
|---|---|---|---|
| 1 | 1,322 | 1,289 | 2,611 |
| 2 | 2,644 | 2,578 | 5,222 |
| 3 | 3,966 | 3,867 | 7,833 |
| 4 | 5,288 | 5,156 | 10,444 |
| 5 | 6,610 | 6,445 | 13,055 |
| 6 | 7,932 | 7,850 | 15,782 |
| 10 | 13,220 | 13,470 | 26,690 |
| 15 | 19,830 | 20,495 | 40,325 |
| 20 | 26,440 | 27,520 | 53,960 |
| 25 | 33,050 | 34,545 | 67,595 |
| 30 | 39,660 | 41,570 | 81,230 |
| 35 | 46,270 | 48,595 | 94,865 |
| 40 | 52,880 | 55,620 | 108,500 |
| 45 | 59,490 | 62,645 | 122,135 |
| 50 | 66,100 | 69,670 | 135,770 |
| 51 | 67,422 | 71,075 | 138,497 |
For a side by side comparison Table 4 shows the estimated lifetime costs.
Table 4
| Category | Patient | Insurance | Insurance + patient |
|---|---|---|---|
| Screening: 50 years | $67,422 | $71,075 | $138,497 |
| Surgery | $5,000 | $89,733 | $94,733 |
Discussion
High risk breast cancer screening has a significant cost. This cost is divided between the patient and the insurance company. In our insurance model, early surgical intervention is the most cost-effective option for the patient as it does not require the continued out of pocket expense of ongoing screening. If a patient has an out pocket maximum of $5,000, she will pay the same amount for surgery as she would for only 4 years of high risk screening. Thus, the earlier she undergoes surgery, the more cost effective surgery becomes. An additional benefit for the patient is the decrease in cancer risk, which screening does not offer. Therefore, the patient gains not only a decreased cancer risk with surgery, they gain an estimated $62,422 in savings from up front surgery versus a lifetime of high risk screening. This is estimated as the total cost of screening for $67,422 minus her out of pocket maximum for surgery. Also the estimate does not include inflation or potential increase in the imaging costs. Other costs which are not included are any biopsies or cancer treatment.
From the insurance company perspective it may seem that high-risk screening alone offers a more cost-effective option. However, the insurance company still pays $71,075 in screening costs. This is only about $20,000 less than the one time surgery costs. Additionally, the insurance company does gain the additional benefit from the risk-reducing surgery arm by decreasing the number of cancers that develop with each diagnosis costing >$75,000 (10).
There are a number of limitations to this study. The first limitation is that there are many insurance plans; however this model allows physicians and patients to help calculate specific costs. Additionally, we do not include the costs of any required second surgeries or potential surgical complications. This cost was not estimated in our analysis in order to decrease the statistical variance of calculating all possible outcomes. Additionally, high risk screening can have the additional cost of unintended false positives and a benign biopsy rate of up to 33% with MRI in this population, quickly driving up costs in the screening arm as well (9). Finally we did not account for different insurance variables, inflation, or differences in out of pocket maximums. The goal was to create a formula by which patients and physicians could calculate and discuss the cost implications of high-risk screening versus prophylactic surgery.
Conclusions
When counseling high risk patients with BRCA 1 or BRCA 2 mutations, it is important to give the patient as much information as possible to allow her to participate in the difficult decision of high risk screening versus prophylactic surgery. Annual high-risk screening with MRI and mammography as well as the additional office visits is costly and time-consuming. In addition to the cost, it is emotionally taxing for women to undergo imaging, office visits, and potential biopsies for any abnormality on imaging. Some patients will elect to have surveillance even with this information, but it is our job to give our patients the most accurate information possible. Over time, the cost will ultimately change and better imaging techniques will become available. As always, we can continue to counsel our on every option so they may make the best personal decisions for their care.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/abs.2018.11.05). The abstract of this work has been published in 2018 Annual Meeting Official Proceedings, Annals of Surgical Oncology. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was IRB approved. Informed consent was waived due to the nature of the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Antoniou A, Pharoah PD, Narod S, et al. Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case Series unselected for family history: a combined analysis of 22 studies. Am J Hum Genet 2003;72:1117-30. [Crossref] [PubMed]
- Johns D, Agarwal J, Anderson L, et al. Breast Cancer Risk Reduction Decisions of the BRCA-Positive Patient: An Observational Study at a Single Institution. J Womens Health (Larchmt) 2017;26:702-6. [Crossref] [PubMed]
- BRCA-Related Breast and/or Ovarian Cancer Syndrome. National Comprehensive Cancer Network (NCCN). Version 2. 2017. Available online: www.nccn.org
- Warner E, Messersmith H, Causer P, et al. Systematic review: using magnetic resonance imaging to screen women at high risk for breast cancer. Ann Intern Med 2008;148:671-9. [Crossref] [PubMed]
- Kriege M, Brekelmans CT, Boetes C, et al. Efficacy of MRI and mammography for breast-cancer screening in women with a familial or genetic predisposition. N Engl J Med 2004;351:427-37. [Crossref] [PubMed]
- Pataky R, Armstrong L, Chia S, et al. Cost-effectiveness of MRI for breast cancer screening in BRCA1/2 mutation carriers. BMC Cancer 2013;13:339. [Crossref] [PubMed]
- Griebsch I, Brown J, Boggis C, et al. Cost-effectiveness of screening with contrast enhanced magnetic resonance imaging vs X-ray mammography of women at a high familial risk of breast cancer. Br J Cancer 2006;95:801-10. [Crossref] [PubMed]
- Rebbeck TR, Friebel T, Lynch HT, et al. Bilateral prophylactic mastectomy reduces breast cancer risk in BRCA1 and BRCA2 mutation carriers: the PROSE Study Group. J Clin Oncol 2004;22:1055-62. [Crossref] [PubMed]
- American College of Radiology ACR Appropriateness Criteria. 2016. Available at Available online: https://acsearch.acr.org/list, accessed September 5, 2018.
- Allaire BT, Ekwueme DU, Guy GP Jr, et al. Medical Care Costs of Breast Cancer in Privately Insured Women Aged 18-44 Years. Am J Prev Med 2016;50:270-7. [Crossref] [PubMed]
Cite this article as: Shirley R, Pastorino A, Lipoff D, Fan B, Halaharvi D, Cripe M. Prophylactic mastectomy can save patients up to $50,000 compared to lifelong screening in BRCA 1 and BRCA 2 patients. Ann Breast Surg 2018;2:20.