The psychological impacts of post-mastectomy breast reconstruction: a systematic review
Highlight box
Key findings
• Breast reconstruction (BR) has been found to be more often beneficial than detrimental to the patient in improving psychologic distress.
• Findings suggest that immediate BR after mastectomy confers greater psychological benefit when compared to delayed BR.
What is known and what is new?
• It is known that BR is a common component of breast cancer treatment.
• Limited literature specifically explores the impacts of different reconstruction methods on psychological distress. This systematic review identifies the impact of various forms of post-mastectomy BR.
What is the implication, and what should change now?
• This study identifies a need for healthcare providers to work to prevent negative mental health outcomes in patients who elect to undergo BR after mastectomy.
• Breast cancer care teams may elect to integrate psychological questioning into their practice in order to assess patient need and promote mental wellbeing throughout the breast cancer journey.
Introduction
Background
Breast cancer is the most common cause of cancer among women and can have a significant impact on both physical and psychological wellbeing (1-3). Treatment for breast cancer typically involves invasive surgical interventions, and in addition to the difficulties intrinsic to experiencing a cancer diagnosis and treatment, undergoing mastectomy can have profound impacts on mental health and self-esteem due to feelings of reduced attractiveness or femininity, changes in self-perception, and negative effects on sexual wellbeing (4). While breast reconstruction (BR) following mastectomy has long been hypothesized to lessen the negative psychological effects of mastectomy by helping to restore a patient’s body image and reducing the toll of cancer surgery on overall mental health, studies on this topic have yielded mixed results (5). As the rates of BR after mastectomy are currently rising in the United States (6), it is vital to develop a comprehensive understanding of how BR influences mental health outcomes.
Rationale and knowledge gap
Factors that can differentiate BR include whether surgery is immediate or delayed, and whether an implant or autologous tissues are used. Some studies have suggested autologous methods yielded higher satisfaction with cosmetic results (7), but there is limited literature that specifically explores the impacts of different reconstruction methods on psychological distress specifically.
Objective
The aim of this systematic review is to explore the effects of BR on postoperative mental health outcomes. We present this article in accordance with the PRISMA reporting checklist (available at https://abs.amegroups.com/article/view/10.21037/abs-23-33/rc).
Methods
Study design and search strategy
A systematic review was conducted on March 10, 2022, using PubMed, Google Scholar, EMBASE, PSYCinfo, and Web of Science databases to identify articles from 1980 to 2022 in accordance with the PRISMA guidelines (8) (Figure 1). An updated search was performed on January 3, 2023, to identify any additional studies. Boolean operators were used to identify articles on BR, and no restrictions were used. The full search strategy may be found in Appendix 1.
Study identification and selection
Articles were included if the full-text article was available, the article was peer-reviewed, all text was written in English, all subjects were humans who underwent BR, and the study used validated instruments to measure psychologic outcomes postoperatively. Articles were excluded if they were non-BR-related, cadaveric/non-human subject studies, commentary/expert opinion/editor’s letter, review articles, or duplicate studies.
Data extraction
The literature searches and initial abstract results were imported and automatically de-duplicated by Covidence (Covidence Ltd, Melbourne, Australia). Two independent reviewers (TL, UA) screened titles and abstracts for inclusion. Any conflicts were resolved by an independent reviewer (MD). Next, the full-text articles were retrieved, and articles were further screened by two independent reviewers (MD, ST) to ensure the initial inclusion criteria were met. A separate independent reviewer (NR) resolved any conflicts. Articles were independently reviewed and assessed for bias and evidence quality. The following data were then extracted from the full-text articles: study title, author, year of publication, country of publication, journal of publication, study design, study aim, study groups, number of patients (and numbers of patients in each group), type of BR, stage of breast-reconstruction, number of times surveyed, questionnaire instruments used, psychologic outcomes, and study conclusions.
Outcomes
The primary outcome of interest was evidence of psychological distress, including a diagnosis of depression, anxiety, post-traumatic stress disorder (PTSD) or other psychiatric disorders. Secondary outcomes included method of testing used to evaluate psychological health, medications, and subsequent treatment. Positive effects on psychologic outcomes were characterized by improved scores on methods of testing, while negative effects on psychologic outcomes were characterized by lower scores on methods of testing.
Data analyses
Data were grouped based on surgical characteristics: mastectomy with breast reconstruction (MBR) versus mastectomy alone (MA), immediate versus delayed BR, and autologous versus implant-based reconstruction. The effect of MBR, immediate reconstruction, and autologous reconstruction were compared to the alternative outcome and directionality on mental health outcomes was determined as “Positive”, “Neutral”, or “Negative”.
Results
A total of 1,644 abstracts were identified, of which 1,388 (84.4%) were excluded. Six full-text articles were unable to be retrieved, leaving 250 available articles that were assessed for eligibility criteria. Of these studies, 151 were excluded for not meeting pre-specified inclusion criteria, due to non-qualifying study outcomes (80.0%), study design (9.3%), or intervention (3.6%). This left 99 studies in the final analysis (Figure 1).
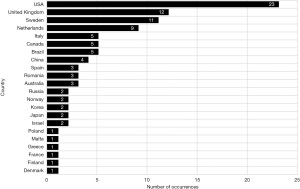
Of these 99 studies, 54 were retrospective and 45 were prospective studies. The most common questionnaire instruments used were the 36-item Short Form Survey (SF-36) (32.3% of studies) and the Hospital Anxiety and Depression Scale (HADS) (30.3%) Authors from the United States published the most articles on this topic (23.2%) followed by the United Kingdom (12.1%), Sweden (11.1%) and the Netherlands (9.1%) (Figure 2).
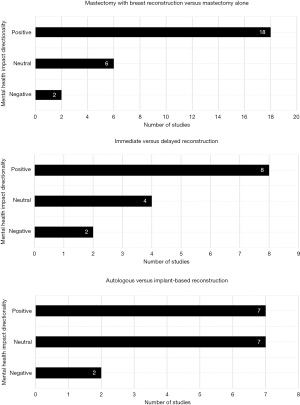
MBR versus MA
In total, 26 studies (26.3%) compared mental health outcomes of patients who had MBR to those who had MA (Table 1). Of these, 18 (69.2%) found that MBR had positive effects on mental health outcomes, 6 (23.1%) found no clear differences, and 2 (7.7%) found negative effects (Figure 3). Of the studies that found women who received MBR to have poorer outcomes, Clark et al. analyzed the psychological effects of BR in a cohort of women who had a history of sexual abuse in childhood. They reported that women in the MBR group reported more distress and greater depressive symptoms than the MA group after controlling for prevalence of abuse (32). The other, Adachi et al. reported that women in the MBR group had a greater tendency towards negative moods compared to patients receiving MA when measured with the Profile of Moods Scale (POMS), and they also reported that the degree of self-efficacy had a marked influence on patient’s moods after surgery (33).
Table 1
| Study authors | Year | Country | Study type | Groups | Total (n) | MBR (n) | MA (n) |
Mental health scales used | Mental health impact: directionality of MBR vs. MA |
|---|---|---|---|---|---|---|---|---|---|
| de Raaff et al. (9) | 2016 | Netherlands | Retrospective cross-sectional | MBR vs. MA | 139 | 34 | 105 | Beck | Positive |
| Li et al. (10) | 2021 | China | Prospective cohort | MBR vs. MA | 152 | 102 | 50 | FACT-B, SAS, SDS | Positive |
| Szadowska-Szlachetka et al. (11) | 2013 | Poland | Retrospective cross-sectional | MBR vs. MA | 241 | 108 | 133 | Beck, EORTC | Positive |
| Tønseth et al. (12) | 2007 | Norway | Retrospective cross-sectional | MBR vs. MA | 58 | 34 | 24 | SF-36 | Positive |
| Fanakidou et al. (13) | 2018 | Greece | Retrospective cross-sectional | MBR vs. MA | 81 | 35 | 46 | DASS-21 | Positive |
| Fortunato et al. (14) | 2021 | Italy | Retrospective cross-sectional | MBR vs. MA | 328 | 172 | 156 | EORTC | Positive |
| Gardikiotis et al. (15) | 2016 | Romania | Retrospective cross-sectional | MBR vs. MA | 50 | 23 | 27 | SF-36 | Positive |
| Ismagilov et al. (16) | 2011 | Russia | Retrospective cross-sectional | MBR vs. MA | 374 | 132 | 242 | SF-36 | Positive |
| Bredicean et al. (17) | 2020 | Romania | Prospective cohort | MBR vs. MA | 64 | 36 | 28 | DASS-21 | Positive |
| Al-Ghazal et al. (18) | 2000 | UK | Retrospective cross-sectional | MBR vs. MA vs. BCS | 577 | 121 | 202 | HADS, RSE | Positive |
| Retrouvey et al. (19) | 2019 | Canada | Prospective cohort | MBR vs. MA vs. BCS | 303 | 70 | 78 | HADS, IES | Positive |
| Archangelo et al. (20) |
2019 | Brazil | Retrospective cross-sectional | MBR vs. MA vs. normal population | 90 | 30 | 30 | Beck | Positive |
| Rubino et al. (21) | 2007 | Italy | Prospective cohort | IBR vs. MA vs. normal pop | 99 | 33 | 33 | HAM-A, HAM-D | Positive |
| Hunsinger et al. (22) | 2016 | France | Retrospective cross-sectional | MBR vs. MA vs. normal population | 3,513 | 70 | 135 | SF-36 | Positive |
| Fernández-Delgado et al. (23) | 2008 | Spain | Retrospective cross-sectional | IBR vs. MA vs. normal pop | 377 | 263 | 114 | HADS, RSE | Positive |
| Pusic et al. (24) | 1999 | USA | Retrospective cross-sectional | MBR vs. MA vs. BCS | 267 | 102 | 71 | SF-36 | Positive |
| Kovačević et al. (25) | 2020 | Russia | Retrospective cross-sectional | MBR vs. MA vs. BCS | 425 | 54 | 256 | WHOQoL-Bref, FACT-B | Positive |
| Pérez-San-Gregorio et al. (26) | 2013 | Spain | Retrospective cross-sectional | MBR vs. MA vs. organ transplant vs. normal population | 706 | 36 | 36 | HADS | Positive |
| Holly et al. (27) | 2003 | UK | Retrospective cross-sectional | MBR vs. MA | 64 | 30 | 34 | HADS, RSE | Neutral |
| Wehrens et al. (28) | 2005 | Netherlands | Retrospective cross-sectional | MBR vs. MA | 222 | 67 | 155 | POMS | Neutral |
| Nicholson et al. (29) | 2007 | UK | Retrospective cross-sectional | MBR vs. MA vs. BCS | 99 | 39 | 46 | HADS, SF-36, DAS-59 | Neutral |
| Harcourt et al. (5) | 2003 | UK | Prospective cohort | Immediate BR vs. delayed BR vs. MA | 103 | 56 | 47 | HADS, EORTC | Neutral |
| Metcalfe et al. (30) | 2012 | Canada | Prospective cohort | Immediate BR vs. delayed BR vs. MA | 190 | 81 | 109 | BSI, IES | Neutral |
| Nano et al. (31) | 2005 | Australia | Retrospective cross-sectional | MBR vs. MA vs. BCS | 310 | 123 | 78 | FACT-B | Neutral |
| Clark et al. (32) | 2011 | UK | Prospective cohort | MBR vs. MA | 133 | 29 | 104 | HADS | Negative |
| Adachi et al. (33) | 2007 | Japan | Retrospective cross-sectional | MBR vs. MA vs. BCS | 102 | 11 | 25 | POMS | Negative |
MBR, mastectomy with breast reconstruction; MA, mastectomy alone; FACT-B, Functional Assessment of Cancer Therapy – Breast; BSI, brief symptom inventory; SAS, Self-rating Anxiety Scale; SDS, Self-rating Depression Scale; EORTC, European Organization for Research and Treatment of Cancer Quality of Life Instruments; SF-36, Short Form – 36 items; DASS-21, Depression, Anxiety, and Stress Scale – 21 items; BCS, breast-conserving surgery; HADS, Hospital Anxiety and Depression Scale; RSE, Rosenberg Self Esteem Scale; IES, Impact of Events Scale; IBR, immediate breast reconstruction; HAM-A, Hamilton Anxiety Ranking Scale; HAM-D, Hamilton Depression Rating Scale; WHOQoL-Bref, World Health Organization Quality of Life Scale Brief Version; POMS, Profile of Mood States; DAS-59, Derriford Appearance Scale 59.
Immediate versus delayed breast reconstruction (DBR)
Fourteen articles examined the effect on psychologic distress of immediate versus DBR (Table 2). Four of these studies (18,34,36,37) (28.6%) found that patients who underwent immediate breast reconstruction (IBR) had better psychologic outcomes compared to those who underwent DBR. In 1985, Wellisch et al. (36) evaluated the psychological differences of women who underwent delayed versus immediate reconstruction and reported women in the IBR group had lower levels of psychological distress and psychological symptoms measured through the Brief Symptom Inventory (BSI). Al-Ghazal et al. (18) found that patients who received IBR had decreased anxiety and depression as well as better scores on body image, self-esteem, and sexual feelings of attractiveness compared to DBR patients. Göktaş et al. (37) and Zhong et al. (34) both demonstrated that patients in the IBR group had a lower prevalence of anxiety and depression compared to the DBR groups.
Table 2
| Study authors | Year | Country | Study type | Groups | Total (n) | Immediate (n) | Delayed (n) | Mental Health scales used | Mental health impact: directionality of immediate vs. delayed |
|---|---|---|---|---|---|---|---|---|---|
| Zhong et al. (34) | 2016 | Canada | Prospective cohort | Immediate vs. delayed | 106 | 30 | 76 | HADS, SF-36 | Positive |
| Atisha et al. (35) | 2008 | USA | Prospective cohort | Immediate vs. delayed | 173 | 116 | 57 | SF-36, FACT-B | Positive |
| Wellisch et al. (36) | 1985 | USA | Retrospective cross-sectional | Immediate vs. delayed | 63 | 25 | 38 | BSI | Positive |
| Fernández-Delgado et al. (23) | 2008 | Spain | Retrospective cross-sectional | Immediate vs. delayed vs. MA | 375 | 194 | 110 | HADS, RSE | Positive |
| Al-Ghazal et al. (18) | 2000 | UK | Retrospective cross-sectional | Immediate vs. delayed | 121 | 38 | 83 | HADS, RSE | Positive |
| Göktaş et al. (37) | 2011 | Israel | Retrospective cross-sectional | Immediate vs. delayed | 51 | 28 | 23 | SCL-R90 | Positive |
| Wilkins et al. (38) | 2000 | USA | Prospective cohort | Compared both immediate vs. delayed, and autologous vs. implant | 273 | 161 | 89 | SF-36, FACT-B | Positive |
| Franchelli et al. (39) | 1995 | Italy | Retrospective cross-sectional | Compared both immediate vs. delayed, and autologous vs. implant | 102 | 34 | 68 | PDI, STAI | Positive |
| Metcalfe et al. (30) | 2012 | Canada | Prospective cohort | Immediate vs. delayed vs. MA | 190 | 24 | 57 | BSI, IES | Neutral |
| Agius et al. (40) | 2016 | Malta | Retrospective cross-sectional | Compared both immediate vs. delayed, and autologous vs. implant | 42 | NA | NA | SF-36 | Neutral |
| Rubino et al. (21) | 2007 | Italy | Prospective cohort | Compared both immediate vs. delayed, and autologous vs. implant | 33 | 21 | 12 | HAM-A, HAM-D | Neutral |
| Juhl et al. (41) | 2017 | Denmark | Retrospective cross-sectional | Immediate vs. delayed | 144 | 27 | 117 | BDI, IES | Neutral |
| Harcourt et al. (5) | 2003 | UK | Prospective cohort | Immediate vs. delayed vs. MA | 103 | 37 | 10 | HADS, EORTC | Negative |
| Roth et al. (42) | 2005 | USA | Prospective cohort | Immediate vs. delayed | 238 | 151 | 87 | SF-36, BSI, FACT-B | Negative |
HADS, Hospital Anxiety and Depression Scale; SF-36, Short Form – 36 items; FACT-B, Functional Assessment of Cancer Therapy – Breast; BSI, Brief Symptom Inventory; RSE, Rosenberg Self Esteem Scale; SCL-R90, Symptom Checklist-90-Revised; PDI, psychological distress inventory; STAI, State Trait Anxiety Inventory; MA, mastectomy alone; IES, Impact of Events Scale; HAM-A, Hamilton Anxiety Ranking Scale; HAM-D, Hamilton Depression Rating Scale; BDI, Beck’s Depression Inventory; EORTC, European Organization for Research and Treatment of Cancer Quality of Life Instruments.
However, the ten other studies (71.4%) found that there were no significant differences between delayed versus immediate BR regarding psychologic outcomes. While the majority of the patients in the study of Fernández-Delgado et al. (23) reported that they had a postprocedural preference for IBR, no significant differences were found between the proportions of immediate versus DBR who were suffering from anxiety or depression. Similarly, Atisha et al. (35) prospectively evaluated 173 patients after mastectomy and found that while there were no significant differences between the delayed and immediate groups, both BR groups had lower anxiety and depression scores compared to the MA group. In contrast, Metcalfe et al. (30) compared patients with MA, IBR and DBR and found no significant differences in psychological functioning.
Autologous versus implant-based breast reconstruction
Sixteen studies (16.2%) compared the psychologic outcomes of autologous versus implant-based reconstruction (Table 3). A wide variety of autologous-based methods were used including deep inferior epigastric perforator (DIEP) flaps (31.3%), transverse rectus abdominis muscle (TRAM) flaps (25%), and latissimus dorsi (LD) flaps (18.8%). Several studies also included a mixed variety of autologous-based methods in their autologous study group (25%).
Table 3
| Study authors | Year | Country | Study design | Total (n) | Implant (n) | Autologous (n) | Type of autologous | Mental health scales used | Mental health impact: directionality of autologous vs. implant-based |
|---|---|---|---|---|---|---|---|---|---|
| Gopie et al. (43) | 2014 | Netherlands | Prospective cohort | 98 | 25 | 73 | DIEP | SF-36, IES | Positive |
| Pusic et al. (44) | 2017 | USA | Prospective cohort | 1,632 | 1,139 | 493 | Mixed | GAD-7, PHQ-9 | Positive |
| Thorarinsson et al. (45) | 2017 | Sweden | Retrospective cross-sectional | 459 | 253 | 206 | DIEP, LD | SF-36, PGWB | Positive |
| Franchelli et al. (39) | 1995 | Italy | Retrospective cross-sectional | 102 | 52 | 50 | TRAM | PDI, STAI | Positive |
| Eltahir et al. (46) | 2015 | Netherlands | Retrospective cross-sectional | 92 | 45 | 47 | Mixed | HADS, SF-36 | Positive |
| Cederna et al. (47) | 1995 | USA | Retrospective cross-sectional | 22 | 14 | 8 | TRAM | FSQ | Positive |
| Winters et al. (48) | 2016 | UK | Prospective cohort | 206 | 93 | 113 | LD | HADS, FACT-B, EORTC | Positive |
| Winters et al. (49) | 2013 | UK | Prospective cohort | 182 | 82 | 100 | LD | HADS, FACT-B, EORTC | Neutral |
| Wilkins et al. (38) | 2000 | USA | Prospective cohort | 250 | 56 | 194 | TRAM | SF-36, FACT-B | Neutral |
| Honkanen et al. (50) | 2021 | Finland | Retrospective cross-sectional | 115 | 10 | 105 | Mixed | HADS, SF-36, BDI | Neutral |
| Agius et al. (40) | 2016 | Malta | Retrospective cross-sectional | 42 | NA | NA | Mixed | SF-36 | Neutral |
| Juhl et al. (41) | 2017 | Denmark | Retrospective cross-sectional | 144 | 49 | 68 | Abdominal flap | BDI, IES | Neutral |
| Tønseth et al. (51) | 2008 | Norway | Retrospective cross-sectional | 64 | 30 | 34 | DIEP | SF-36 | Neutral |
| Rubino et al. (21) | 2007 | Italy | Prospective cohort | 33 | 16 | 17 | TRAM | HAM-A, HAM-D | Neutral |
| Timman et al. (52) | 2017 | Netherlands | Prospective cohort | 114 | 69 | 75 | DIEP | HADS, IES | Negative |
| Gopie et al. (53) | 2013 | Netherlands | Retrospective cross-sectional | 150 | 64 | 86 | DIEP | HADS, IES | Negative |
DIEP, Deep inferior epigastric perforator flap; SF-36, Short Form – 36 items; IES, Impact of Events Scale; GAD-7, Generalized Anxiety Disorder 7-Item Scale; PHQ-9, Patient Health Questionnaire-9; LD, latissimus dorsi flap; PGWB, Psychological General Well-Being Index; TRAM, transverse rectus abdominis muscle flap; PDI, Psychological Distress Inventory; STAI, State Trait Anxiety Inventory; HADS, Hospital Anxiety and Depression Scale; FSQ, Functional Status Questionnaire; FACT-B, Functional Assessment of Cancer Therapy – Breast; EORTC, European Organization For Research and Treatment of Cancer Quality of Life Instruments; BDI, Beck’s Depression Inventory; HAM-A, Hamilton Anxiety Ranking Scale; HAM-D, Hamilton Depression Rating Scale.
Overall, there were mixed results when comparing the effects of autologous and implant-based methods on psychological distress (Figure 3). While eight studies (40,41,44-47,51,52) (50.0%) reported patients receiving autologous BR were more satisfied with the results of their breast appearance and feel, none of these studies reported that autologous BR had a significantly superior effect on psychological wellbeing compared to implant-based reconstruction. Tønseth et al. (51) evaluated 64 women undergoing BR with either DIEP or expandable breast implants and found that those in the DIEP group were more satisfied with appearance, reported improved social relationships and were less concerned with negative body image, but no significant differences in any of the SF-36 measures, including the mental health subscale, were reported. Eltahir et al. (46) had similar findings that while women who had autologous BR were more likely to be more satisfied with their breasts, there were no significant differences regarding psychological distress. Interestingly, Pusic et al. (44) found that patients who underwent autologous BR had a significantly greater psychosocial wellbeing 1 year postoperatively measured by the BREAST-Q but did not have any significant differences regarding mental health outcomes such as anxiety, depression, or sleep disturbances. The BREAST-Q is a widely used questionnaire to evaluate patients’ psychosocial wellbeing after breast reconstruction and is one popular method used to evaluate patient post-operative satisfaction and effect on quality of life. While not used as an overt measure of mental health outcomes, it may be used as a proxy to measure psychological wellbeing. Lastly, Thorarinsson et al. (45) compared implant-based BR with three autologous methods (DIEP, LD, lateral thoracodorsal flap) and found that while DIEP BR patients were the most satisfied with their reconstruction results, none of the groups had significant differences in psychologic outcomes.
Three studies (18.8%) reported that autologous BR methods were associated with worse psychologic outcomes. In 1995, Franchelli et al. (39) reported that both autologous and implant-based reconstruction groups indicated lower psychological distress overall, but in comparison, TRAM flap patients had more relevant psychological discomfort than implant BR patients. More recently, Winters et al. (49) also found that patients who underwent autologous LD operations had greater levels of anxiety 2 and 3 years postoperatively compared to the implant-assisted group. Gopie et al. (43) found that both the autologous and implant groups in their study had less cancer-specific distress. However, while implant BR patients had less anxiety postoperatively, DIEP BR patients exhibited more depressive symptoms. This study also noted that patients with surgical complications had an increased likelihood of both anxiety and depressive symptoms, especially DIEP BR patients, who reported depressive scores of clinical concern. The five other studies (31.3%) found comparable psychologic outcomes when comparing autologous and implant-based BR methods. Gopie et al. (43) found that both implant and DIEP groups had comparable scores for both cancer distress and psychologic outcomes.
Early complications worsen psychologic outcomes in short-term follow-ups
Four studies found that early postoperative complications were associated with worse psychologic outcomes (49,53-55). Gopie et al. (43) found that the presence of complications in both implant and autologous BR groups increased depressive and anxious symptoms and DIEP BR patients had depressive symptoms of clinical concern when the surgery was followed by complications. Lu et al. (55) followed only autologous BR patients and found that 58% of the cohort had postoperative complications and complications were associated with decreased psychologic scores in early follow-ups months after the surgery. However, at the one-year follow up, the psychologic scores returned to baseline. den Heijer et al. (54) reported a similar finding that complications worsened depressive outcomes in both implant and autologous groups in short-term follow-ups but at the 21-month follow-up, depressive scores generally declined to normal levels for both groups. Momoh et al. (56) compared the complication rates and psychologic outcomes between patients undergoing either bilateral or unilateral breast reconstruction surgeries. They found that despite bilateral reconstruction patients having higher rates of early complications compared to unilateral reconstruction patients, patients who received bilateral surgeries still had lower anxiety scores at the 1-year follow-up.
Discussion
MBR versus MA
Our review identified several studies that demonstrate higher scores on psychologic wellbeing questionnaires following mastectomy and breast reconstruction when compared to mastectomy alone. A recent meta-analysis evaluating the psychological impacts of breast reconstruction found that women who had MBR had significantly decreased incidences of anxiety and depression compared to women who had MA (57). Other studies have concluded that BR is beneficial in improving perceptions of body image (38) and improving overall mental health postoperatively (13). However, these findings are directly challenged by results of studies evaluated in our analysis, which reported higher levels of distress and negative mood in patients who underwent MBR (32,33). It is important to note the study design and population of the studies which revealed a negative association with wellbeing and MBR. Of the two studies that concluded that MBR was associated with distress and negative moods, the first was conducted in a population of patients who had endured sexual abuses at a young age. This is not a representative sample of the entire population of patients who elect to undergo MBR. The second study utilized the POMS, a scale that measures transient mood states rather than enduring symptoms of mood dysregulation. A lack of standardization of data capture materials across studies and differences in patient selection may contribute to the heterogeneity of the data. Future studies may benefit from conducting a meta-analysis of the available literature.
Immediate versus delayed
Our review identified studies comparing the psychological benefits of immediate versus delayed reconstruction that demonstrated mixed results. Some suggest immediate BR may be more beneficial to protect mental health while others did not report a significant difference in psychological outcomes between IBR and DBR. Our findings in this study echo prior research that concluded that patients who underwent IBR after mastectomy had significantly less recalled distress about their mastectomy than those who underwent delayed reconstruction (58). It is possible that IBR is favorable for reducing psychologic distress, as the patient may not feel that any part of them was removed for a significant period of time. Patients are not subjected to an additional procedure at a later date, meaning there is one less trip to the hospital and any emotional distress or pain that may lead up to it. The option for both immediate versus delayed breast reconstruction is available to patients when evaluating breast reconstructive options, and while post-operative complications are primarily discussed when coming to a decision, patients may benefit from a fuller understanding of the psychosocial effects of either option.
Autologous versus implant
Patients are presented with two reconstructive options following mastectomy: autologous and implant-based breast reconstruction. While patients experienced higher levels of satisfaction with the appearance of their breasts following autologous reconstruction compared to implant-based reconstruction (51), there is no consensus regarding whether one type yielded more psychological benefits or detriments than the other. A multitude of variables influence the operative experience for patients who undergo breast reconstructive procedures following mastectomy. Complications following reconstructive surgery may be a factor that influences patient’s wellbeing. While complication rates and characteristics vary among procedures, studies comparing patients who elect to undergo autologous breast reconstruction have a significantly higher odds of developing any complication compared with those undergoing expander-implancbased reconstruction (59). It is a possibility that patients who undergo autologous breast reconstruction are faced with more postoperative challenges, such as flap necrosis or flap loss, that may influence their mental wellbeing for up to several years after their procedures. Further, studies were limited in their analysis of the type of autologous reconstruction and psychologic outcomes. Sub-analysis of autologous reconstruction type may reveal novel findings.
Limitations of review
In this study, it is possible that relevant questionnaires were excluded from the inclusion criteria or the screening processes. Furthermore, the scope of this systematic review is restricted by the limited number of widely accepted and validated questionnaires that address patient psychologic health directly and appropriately. As a limiting factor of this systematic review, it is important for further studies to utilize specific tools that directly assess patient psychologic health in patients undergoing breast reconstruction.
Finally, this review included only articles written in English. While some of the validated surveys included in this systematic review are validated in other languages, some are not. This has the potential to exclude data that could have impacted results in a meaningful way due to the fact that different cultures using different languages may have variations in the way that mental health is understood or would be expressed in a survey (60). Excluding for English-only studies, however, allowed homogeneity in studies that were considered for inclusion.
Culturally competent survey interpretation
It is important to understand the results of this systematic review using a lens of cultural competency. The different countries from which each of the studies included in this systematic review are from all have their own unique cultures. These individual cultures can contribute to variations in the way that the patients completing these surveys regarding their mental health following breast reconstruction chose not only how to communicate their symptoms but also which to report. Each individual country has a culture that is imbued with specific meanings, values, and understandings of mental health and wellbeing. In this way, culture and the geographic makeup of the studies included in this study may serve as potential confounders in our systematic review. However, while there is heterogeneity in the country of origin in which the studies included in this systematic review were conducted, the inclusion of studies from 22 different countries suggests that the results of this systematic review are more representative of a broader range and demographic of patients.
Selection bias
As this systematic review analyzes studies that use patient-based and patient-reported instruments to measure mental health outcomes, there is the potential that these studies, and therefore, this systematic review, selected only for patients who were likely to complete these mental health questionnaires. Research involving survey has continuously been challenged because of issues of selection bias and gaining results from non-responders (61,62). Future research should work to either minimize the potential of selection bias or better account for this potential confounder in order to optimize studies utilizing surveys as a primary source of data collection (62). This selection bias, however, could potentially reflect similar patterns that are seen in the biased patterns of individuals seeking out mental healthcare. Multiple studies have shown that mental healthcare utilization and treatment seeking behaviors differ greatly between varying patient populations for many reasons (63,64). It is therefore possible that those who seek out mental health care would be more likely to complete surveys regarding the same topic.
Implications and actions needed
Given the findings of this study, the authors propose that healthcare practitioners can play a role in preventing negative mental health outcomes in patients who elect to undergo breast reconstruction after mastectomy. A thorough assessment of the psychological status of a patient prior to breast reconstruction using a clinically validated tool is a first step toward understanding how to address mental health needs in patients who receive such a life-altering procedure.
Conclusions
Breast reconstruction has been found to be more often beneficial than detrimental to the patient in improving psychologic distress after surgery. This is the first systematic review to date that analyzes the psychological wellbeing of patients undergoing breast reconstruction after mastectomy by subdividing studies based on reconstruction type and temporality of the reconstruction procedure. Future work is needed to discern if the specific type of BR influences postoperative psychological wellbeing.
Acknowledgments
Funding: The study was supported by the National Cancer Institute of the National Institutes of Health (Award Number R25CA236636; to J.B.S.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://abs.amegroups.com/article/view/10.21037/abs-23-33/rc
Peer Review File: Available at https://abs.amegroups.com/article/view/10.21037/abs-23-33/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://abs.amegroups.com/article/view/10.21037/abs-23-33/coif). J.B.S. was supported by the National Cancer Institute of the National Institutes of Health (Award Number R25CA236636). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Fann JR, Thomas-Rich AM, Katon WJ, et al. Major depression after breast cancer: a review of epidemiology and treatment. Gen Hosp Psychiatry 2008;30:112-26. [Crossref] [PubMed]
- Somerset W, Stout SC, Miller AH, et al. Breast cancer and depression. Oncology (Williston Park) 2004;18:1021-34; discussion 1035-6, 1047-8.
- Burgess C, Cornelius V, Love S, et al. Depression and anxiety in women with early breast cancer: five year observational cohort study. BMJ 2005;330:702. [Crossref] [PubMed]
- Koçan S, Gürsoy A. Body Image of Women with Breast Cancer After Mastectomy: A Qualitative Research. J Breast Health 2016;12:145-50. [Crossref] [PubMed]
- Harcourt DM, Rumsey NJ, Ambler NR, et al. The psychological effect of mastectomy with or without breast reconstruction: a prospective, multicenter study. Plast Reconstr Surg 2003;111:1060-8. [Crossref] [PubMed]
- Albornoz CR, Bach PB, Mehrara BJ, et al. A paradigm shift in U.S. Breast reconstruction: increasing implant rates. Plast Reconstr Surg 2013;131:15-23. [Crossref] [PubMed]
- Toyserkani NM, Jørgensen MG, Tabatabaeifar S, et al. Autologous versus implant-based breast reconstruction: A systematic review and meta-analysis of Breast-Q patient-reported outcomes. J Plast Reconstr Aesthet Surg 2020;73:278-85. [Crossref] [PubMed]
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. [Crossref] [PubMed]
- de Raaff CA, Derks EA, Torensma B, et al. Breast reconstruction after mastectomy: does it decrease depression at the long-term? Gland Surg 2016;5:377-84. [Crossref] [PubMed]
- Li YJ, Tang XN, Li XQ. Effect of modified radical mastectomy combined with latissimus dorsi musculocutaneous flap breast reconstruction on patients' psychology and quality of life. Am J Transl Res 2021;13:11548-55. [PubMed]
- Szadowska-Szlachetka ZC, Stanislawek A, Kachaniuk H, et al. Occurrence of depression symptoms measured by the Beck Depression Inventory (BDI) in women after mastectomy and breast reconstruction with regard to the assessment of quality of life. Przegląd Menopauzalny 2013;12:293-9.
- Tønseth KA, Hokland BM, Tindholdt TT, et al. Patient-reported outcomes after breast reconstruction with deep inferior epigastric perforator flaps. Scand J Plast Reconstr Surg Hand Surg 2007;41:173-7. [Crossref] [PubMed]
- Fanakidou I, Zyga S, Alikari V, et al. Mental health, loneliness, and illness perception outcomes in quality of life among young breast cancer patients after mastectomy: the role of breast reconstruction. Qual Life Res 2018;27:539-43. [Crossref] [PubMed]
- Fortunato L, Loreti A, Cortese G, et al. Regret and Quality of Life After Mastectomy With or Without Reconstruction. Clin Breast Cancer 2021;21:162-9. [Crossref] [PubMed]
- Gardikiotis I, Azoicai D, Dobreanu C, et al. Socio-Epidemiological Points of View Regarding Quality Of Life in Patients With and Without Breast Reconstruction after Mastectomy for Cancer. Revista de Cercetare si Interventie Sociala 2016;52:92-104.
- Ismagilov AK, Khasanov RS, Navrusov SN, et al. Study on possibilities of reconstructive--plastic surgery in patients with stage III breast cancer. Bratisl Lek Listy 2011;112:686-90. [PubMed]
- Bredicean AC, Crăiniceanu Z, Oprean C, et al. The influence of cognitive schemas on the mixed anxiety-depressive symptoms of breast cancer patients. BMC Womens Health 2020;20:32. [Crossref] [PubMed]
- Al-Ghazal SK, Fallowfield L, Blamey RW. Comparison of psychological aspects and patient satisfaction following breast conserving surgery, simple mastectomy and breast reconstruction. Eur J Cancer 2000;36:1938-43. [Crossref] [PubMed]
- Retrouvey H, Kerrebijn I, Metcalfe KA, et al. Psychosocial Functioning in Women with Early Breast Cancer Treated with Breast Surgery With or Without Immediate Breast Reconstruction. Ann Surg Oncol 2019;26:2444-51. [Crossref] [PubMed]
- Archangelo SCV, Sabino Neto M, Veiga DF, et al. Sexuality, depression and body image after breast reconstruction. Clinics (Sao Paulo) 2019;74:e883. [Crossref] [PubMed]
- Rubino C, Figus A, Lorettu L, et al. Post-mastectomy reconstruction: a comparative analysis on psychosocial and psychopathological outcomes. J Plast Reconstr Aesthet Surg 2007;60:509-18. [Crossref] [PubMed]
- Hunsinger V, Hivelin M, Derder M, et al. Long-Term Follow-Up of Quality of Life following DIEP Flap Breast Reconstruction. Plast Reconstr Surg 2016;137:1361-71. [Crossref] [PubMed]
- Fernández-Delgado J, López-Pedraza MJ, Blasco JA, et al. Satisfaction with and psychological impact of immediate and deferred breast reconstruction. Ann Oncol 2008;19:1430-4. [Crossref] [PubMed]
- Pusic A, Thompson TA, Kerrigan CL, et al. Surgical options for the early-stage breast cancer: factors associated with patient choice and postoperative quality of life. Plast Reconstr Surg 1999;104:1325-33. [Crossref] [PubMed]
- Kovačević P, Miljković S, Višnjić A, et al. Quality of Life Indicators in Patients Operated on for Breast Cancer in Relation to the Type of Surgery-A Retrospective Cohort Study of Women in Serbia. Medicina (Kaunas) 2020;56:402. [Crossref] [PubMed]
- Pérez-San-Gregorio MA, Fernández-Jiménez E, Martín-Rodríguez A, et al. Quality of life in women following various surgeries of body manipulation: organ transplantation, mastectomy, and breast reconstruction. J Clin Psychol Med Settings 2013;20:373-82. [Crossref] [PubMed]
- Holly P, Kennedy P, Taylor A, et al. Immediate breast reconstruction and psychological adjustment in women who have undergone surgery for breast cancer: a preliminary study. Psychol Health Med 2003;8:441-52. [Crossref] [PubMed]
- Wehrens KME, Cuypers WJSS, Boeckx WD, et al. Psychological profile of women seeking breast reconstruction and quality of life assessment after surgery. Eur J Plast Surg 2005;28:264-7. [Crossref]
- Nicholson RM, Leinster S, Sassoon EM. A comparison of the cosmetic and psychological outcome of breast reconstruction, breast conserving surgery and mastectomy without reconstruction. Breast 2007;16:396-410. [Crossref] [PubMed]
- Metcalfe KA, Semple J, Quan ML, et al. Changes in psychosocial functioning 1 year after mastectomy alone, delayed breast reconstruction, or immediate breast reconstruction. Ann Surg Oncol 2012;19:233-41. [Crossref] [PubMed]
- Nano MT, Gill PG, Kollias J, et al. Psychological impact and cosmetic outcome of surgical breast cancer strategies. ANZ J Surg 2005;75:940-7. [Crossref] [PubMed]
- Clark L, Holcombe C, Hill J, et al. Sexual abuse in childhood and postoperative depression in women with breast cancer who opt for immediate reconstruction after mastectomy. Ann R Coll Surg Engl 2011;93:106-10. [Crossref] [PubMed]
- Adachi K, Ueno T, Fujioka T, et al. Psychosocial factors affecting the therapeutic decision-making and postoperative mood states in Japanese breast cancer patients who underwent various types of surgery: body image and sexuality. Jpn J Clin Oncol 2007;37:412-8. [Crossref] [PubMed]
- Zhong T, Hu J, Bagher S, et al. A Comparison of Psychological Response, Body Image, Sexuality, and Quality of Life between Immediate and Delayed Autologous Tissue Breast Reconstruction: A Prospective Long-Term Outcome Study. Plast Reconstr Surg 2016;138:772-80. [Crossref] [PubMed]
- Atisha D, Alderman AK, Lowery JC, et al. Prospective analysis of long-term psychosocial outcomes in breast reconstruction: two-year postoperative results from the Michigan Breast Reconstruction Outcomes Study. Ann Surg 2008;247:1019-28. [Crossref] [PubMed]
- Wellisch DK, Schain WS, Noone RB, et al. Psychosocial correlates of immediate versus delayed reconstruction of the breast. Plast Reconstr Surg 1985;76:713-8. [Crossref] [PubMed]
- Göktaş SB, Güllüoğlu BM, Şelimen D. Immediate or delayed breast reconstruction after radical mastectomy in breast cancer patients: Does it make a difference in the quality of life. Turk. Klin. Tip Bilimleri Derg 2011;31:664-73. [Crossref]
- Wilkins EG, Cederna PS, Lowery JC, et al. Prospective analysis of psychosocial outcomes in breast reconstruction: one-year postoperative results from the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg 2000;106:1014-25; discussion 1026-7. [Crossref] [PubMed]
- Franchelli S, Leone MS, Berrino P, et al. Psychological evaluation of patients undergoing breast reconstruction using two different methods: autologous tissues versus prostheses. Plast Reconstr Surg 1995;95:1213-8; discussion 1219-20. [Crossref] [PubMed]
- Agius M, Camilleri L, Galea J. The physical and psychological effects of breast reconstruction in breast cancer patients. A retrospective quantitative analysis between 2009 and 2011 at Mater Dei Hospital, Malta. Hellenic J Surg 2016;88:79-84. [Crossref]
- Juhl AA, Christensen S, Zachariae R, et al. Unilateral breast reconstruction after mastectomy - patient satisfaction, aesthetic outcome and quality of life. Acta Oncol 2017;56:225-31. [Crossref] [PubMed]
- Roth RS, Lowery JC, Davis J, et al. Quality of life and affective distress in women seeking immediate versus delayed breast reconstruction after mastectomy for breast cancer. Plast Reconstr Surg 2005;116:993-1002; discussion 1003-5. [Crossref] [PubMed]
- Gopie JP, ter Kuile MM, Timman R, et al. Impact of delayed implant and DIEP flap breast reconstruction on body image and sexual satisfaction: a prospective follow-up study. Psychooncology 2014;23:100-7. [Crossref] [PubMed]
- Pusic AL, Matros E, Fine N, et al. Patient-Reported Outcomes 1 Year After Immediate Breast Reconstruction: Results of the Mastectomy Reconstruction Outcomes Consortium Study. J Clin Oncol 2017;35:2499-506. [Crossref] [PubMed]
- Thorarinsson A, Fröjd V, Kölby L, et al. Long-Term Health-Related Quality of Life after Breast Reconstruction: Comparing 4 Different Methods of Reconstruction. Plast Reconstr Surg Glob Open 2017;5:e1316. [Crossref] [PubMed]
- Eltahir Y, Werners LLCH, Dreise MM, et al. Which breast is the best? Successful autologous or alloplastic breast reconstruction: patient-reported quality-of-life outcomes. Plast Reconstr Surg 2015;135:43-50. [Crossref] [PubMed]
- Cederna PS, Yates WR, Chang P, et al. Postmastectomy reconstruction: comparative analysis of the psychosocial, functional, and cosmetic effects of transverse rectus abdominis musculocutaneous flap versus breast implant reconstruction. Ann Plast Surg 1995;35:458-68. [Crossref] [PubMed]
- Winters ZE, Afzal M, Balta V, et al. Patient-reported outcomes and their predictors at 2- and 3-year follow-up after immediate latissimus dorsi breast reconstruction and adjuvant treatment. Br J Surg 2016;103:524-36. [Crossref] [PubMed]
- Winters ZE, Haviland J, Balta V, et al. Integration of patient-reported outcome measures with key clinical outcomes after immediate latissimus dorsi breast reconstruction and adjuvant treatment. Br J Surg 2013;100:240-51. [PubMed]
- Honkanen N, Mustonen L, Kalso E, et al. Breast reconstruction after breast cancer surgery - persistent pain and quality of life 1-8 years after breast reconstruction. Scand J Pain 2021;21:522-9. [Crossref] [PubMed]
- Tønseth KA, Hokland BM, Tindholdt TT, et al. Quality of life, patient satisfaction and cosmetic outcome after breast reconstruction using DIEP flap or expandable breast implant. J Plast Reconstr Aesthet Surg 2008;61:1188-94. [Crossref] [PubMed]
- Timman R, Gopie JP, Brinkman JN, et al. Most women recover from psychological distress after postoperative complications following implant or DIEP flap breast reconstruction: A prospective long-term follow-up study. PLoS One 2017;12:e0174455. [Crossref] [PubMed]
- Gopie JP, Timman R, Hilhorst MT, et al. The short-term psychological impact of complications after breast reconstruction. Psychooncology 2013;22:290-8. [Crossref] [PubMed]
- den Heijer M, Seynaeve C, Timman R, et al. Body image and psychological distress after prophylactic mastectomy and breast reconstruction in genetically predisposed women: a prospective long-term follow-up study. Eur J Cancer 2012;48:1263-8. [Crossref] [PubMed]
- Lu SM, Nelson JA, Fischer JP, et al. The impact of complications on function, health, and satisfaction following abdominally based autologous breast reconstruction: a prospective evaluation. J Plast Reconstr Aesthet Surg 2014;67:682-92. [Crossref] [PubMed]
- Momoh AO, Cohen WA, Kidwell KM, et al. Tradeoffs Associated With Contralateral Prophylactic Mastectomy in Women Choosing Breast Reconstruction: Results of a Prospective Multicenter Cohort. Ann Surg 2017;266:158-64. [Crossref] [PubMed]
- Chen W, Lv X, Xu X, et al. Meta-analysis for psychological impact of breast reconstruction in patients with breast cancer. Breast Cancer 2018;25:464-9. [Crossref] [PubMed]
- Schain WS, Wellisch DK, Pasnau RO, et al. The sooner the better: a study of psychological factors in women undergoing immediate versus delayed breast reconstruction. Am J Psychiatry 1985;142:40-6. [Crossref] [PubMed]
- Bennett KG, Qi J, Kim HM, et al. Comparison of 2-Year Complication Rates Among Common Techniques for Postmastectomy Breast Reconstruction. JAMA Surg 2018;153:901-8. [Crossref] [PubMed]
- Slama K, Chiang CY, Enarson DA, et al. Tobacco and tuberculosis: a qualitative systematic review and meta-analysis. Int J Tuberc Lung Dis 2007;11:1049-61. [PubMed]
- Compton J, Glass N, Fowler T. Evidence of Selection Bias and Non-Response Bias in Patient Satisfaction Surveys. Iowa Orthop J 2019;39:195-201. [PubMed]
- Frobeen AL, Kowalski C, Weiß V, et al. Investigating Respondents and Nonrespondents of a Postal Breast Cancer Questionnaire Survey Regarding Differences in Age, Medical Conditions, and Therapy. Breast Care (Basel) 2016;11:139-43. [Crossref] [PubMed]
- Karadag O, Kilic C, Kaya E, et al. Challenges and lessons learned in mental health research among refugees: a community-based study in Turkey. BMC Public Health 2021;21:1537. [Crossref] [PubMed]
- Woodall A, Morgan C, Sloan C, et al. Barriers to participation in mental health research: are there specific gender, ethnicity and age related barriers? BMC Psychiatry 2010;10:103. [Crossref] [PubMed]
Cite this article as: Roy N, Downes MH, Ibelli T, Amakiri UO, Li T, Tebha SS, Balija TM, Schnur JB, Montgomery GH, Henderson PW. The psychological impacts of post-mastectomy breast reconstruction: a systematic review. Ann Breast Surg 2024;8:19.