
Corrective surgeries following prophylactic and therapeutic mastectomy with immediate breast reconstruction
Introduction
Breast cancer is one of the most frequent types of cancer affecting one in 10 women. The survival rates have been increasing since 1989 (1). This has resulted in an increased demand for breast reconstruction. During the last decade, new methods using different types of mesh have enabled a simplified immediate breast reconstruction using direct to implant methods in women eligible for mastectomy (2). The new methods have improved the aesthetic results leading to an increased demand for breast reconstruction following both therapeutic and prophylactic mastectomy (3).
Women facing a breast cancer diagnosis or the decisions surrounding a prophylactic procedure due to high risk of breast cancer have multiple factors to consider in regard to treatment. The decision to have a simple mastectomy or a direct to implant breast reconstruction would be based on expected cosmetic and functional results, oncologic safety as well as risk of complications. Furthermore, the risk of additional procedures in order to achieve a satisfying cosmetic result might be a substantial consideration for the patient.
Corrective surgeries following mastectomy and immediate breast reconstruction includes release and removal of scar tissue, change of implant size, shape or profile due to asymmetry of volume, displacement of implant, rippling, capsular formation, breast animation or correction of the contralateral natural breast. The number and degree of reoperations is a decision made by the patient and the surgeon in collaboration. It depends, however, on an individual balance between the patients wish for optimal cosmetic result and the amount of effort the woman is willing to offer.
Both breast cancer patients and prophylactically treated women might suffer from common psychological side effects following reconstruction as changes in body appearance, feelings of femininity and sexual relationships (4,5). Breast cancer patients have additionally been found to experience poor-emotional well-being, depressive symptomatology, breast cancer specific concerns, and impaired social functioning (6). These consequences may impact the choice of breast cancer patients to have corrective surgery following direct to implant reconstruction.
A thorough review of the need for corrective procedures following mastectomy and direct to implant breast reconstruction among cancer patients and prophylactically treated women has not yet been definitively explored in the literature. The aim of this study was to cast light on the frequency and types of corrective surgeries in women treated with therapeutic mastectomy and direct to implant breast reconstruction and women treated with prophylactic mastectomy and direct to implant breast reconstruction.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/abs-20-63).
Methods
Study design, setting and population
A retrospective review of patients who underwent either therapeutic or prophylactic mastectomy and direct to implant reconstruction by the same senior surgeon during January 1st 2014 and December 31st 2017 at the Department of Plastic Surgery, Odense University Hospital was undertaken. Of the 122 identified patients, 67 patients had received a therapeutic mastectomy and 55 had received a prophylactic mastectomy. Patients were defined as cancer patients if at any point cancer was detected in either breast. Prophylactic patients were never diagnosed with breast cancer. Both prophylactic and cancer patients underwent the same mastectomy technique with hydro dissection and careful dissection of the mastectomy skin flaps when primary reconstruction was planned. Our surgical group uses a combination of pre-operative and operative techniques to minimize reoperations. All patients are carefully measured, and a breast footprint is drawn before surgery. The footprint is used in surgery along with skin flap thickness to evaluate the suitable implant size. Atraumatic dissection technique with hydro dissection and scissor reduce trauma and helps maintain good perfusion, ultimately minimizing reoperations.
Data collection
Primary outcome was number of corrective surgeries for the two different groups of women. Secondary outcomes were indication and types of corrective surgeries the women underwent. Additionally, data on possible confounders as age, body mass index (BMI), smoking, hypertension, diabetes and other comorbidities, data related to surgical procedures including implant size, shape and placement, surgical procedure and the number of hospitalization days following the procedure were obtained from medical charts.
Patients were followed from date of surgery until the 1st of October 2018. In this period, all corrective surgery occurring after the primary surgery was registered. Nipple reconstruction and tattooing of the areola was omitted. The end point of this reconstructive process for any individual woman was a decision made between the woman and the single senior surgeon.
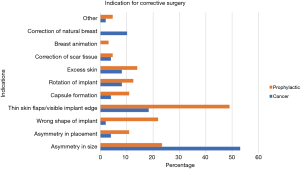
The indications were categorized into 11 categories as follows: correction of contralateral natural breast, breast animation, correction of scar tissue, excess skin, rotation of implant, capsule formation, thin skin flaps/visible implant, wrong shape of implant, asymmetry in placement, asymmetry in size and other. Study data were collected and managed using REDCap electronic data capture tools hosted at Odense University Hospital (Research Electronic Data Capture) (7).
Statistical analysis
Chi-square and Fisher’s exact test were used to compare the proportion of women experiencing corrective surgeries in the prophylactic group compared to the therapeutic group as well as the proportion of patients with comorbidities.
To explore if there was a significant difference in the number of corrective surgeries between the two groups, we first applied negative binomial regression, and, as the result showed no signs of overdispersion, we then applied Poisson regression for a more accurate result.
Baseline characteristics were presented for the 122 women. Student’s t-test and Fisher’s exact test were used to examine differences in age and BMI between groups.
All statistical analysis was conducted using Stata/IC 15.0 for Mac (StataCorp., 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp. LLC). P values <0.05 were considered statistically significant.
Ethics
The study was approved by the Danish Patient Safety Authority (3-3013-2117/1) and The Danish Data Protection Agency (17/15192). The study was conducted in accordance with the declaration of Helsinki (as revised in 2013) and informed consent was taken from all the patients.
Results
Baseline characteristics
Patient characteristics are presented in Table 1. There was a significant difference in age between the prophylactic and the therapeutically treated women; 39.7 years compared to 50.1 years (P<0.001). There was a significant larger percentage of patients with hypertension in the therapeutic group 9/67 (13%) compared to the prophylactic group 0/55 (0%) (P=0.004).
Table 1
| Characteristics | Total (n=122) | Cancer (n=67) | Prophylactic (n=55) | P value |
|---|---|---|---|---|
| Age (years), mean ± SD | 45.4±11.1 | 50.1±10.8 | 39.7±8.3 | <0.001 |
| BMI (kg/m2), n (%) | 0.016 | |||
| <18.5 | 1 (0.8) | 1 (1.5) | 0 (0.0) | |
| 18.5–25 | 52 (42.6) | 25 (37.3) | 27 (49.1) | |
| 25–30 | 22 (18.0) | 8 (11.9) | 14 (25.5) | |
| >30 | 47 (38.5) | 33 (49.3) | 14 (25.5) | |
| Mean ± SD | 24.6±4.4 | 24.2±4.4 | 25.2±4.4 | 0.211 |
| Smoking, n (%) | 0.802 | |||
| Yes | 12 (9.8) | 7 (10.5) | 5 (9.1) | |
| No | 110 (90.2) | 60 (89.5) | 50 (90.9) | |
| Hypertension, n (%) | 0.004 | |||
| Yes | 9 (7.4) | 9 (13.4) | 0 (0.0) | |
| No | 113 (92.6) | 58 (86.6) | 55 (100.0) | |
| Diabetes, n (%) | 0.065 | |||
| Yes | 4 (3.3) | 4 (6.0) | 0 (0.0) | |
| No | 118 (96.7) | 63 (94.0) | 55 (100.0) | |
| Other comorbidities, n (%) | 0.080 | |||
| Yes | 13 (10.7) | 10 (14.9) | 3 (5.5) | |
| No | 109 (89.4) | 57 (85.1) | 52 (94.5) | |
| Treatment, n (%) | ||||
| Adjuvant chemotherapy | 18 (26.9) | |||
| Anti-hormone therapy | 12 (17.9) | |||
| Radiation therapy | 2 (3.0) | |||
| Other treatment | 0 (0.0) | |||
| No treatment | 35 (52.2) |
BMI, body mass index.
Oncologic and reconstruction characteristics
In both groups, patients were discharged on average 3.8 days after surgery. The implant size was larger in the prophylactic group (440 cc) compared to the cancer group (363 cc) (P=0.002). No difference was found between the two groups regarding implant placement or shape of the implant. Subpectoral placement was chosen in most cases (88%), as was anatomical shape (97%) (Table 2). Most implants were microtextured. Forty percent of all patients had nipple-sparing mastectomy and 61% had skin-sparing mastectomy (P<0.001). Figures 1,2 shows a therapeutic and prophylactic patient after bilateral mastectomy, one with the removal of nipple-areola-complex and one with only removal of the nipple. The prophylactic patient was corrected once.
Table 2
| Surgical data | Total (n=122) | Cancer* (n=67) | Prophylactic (n=55) | P value |
|---|---|---|---|---|
| Hospitalization (days) | 3.8±2.4 | 3.6±2.2 | 4.2±2.5 | 0.165 |
| Implant size (mL) | 398.4±135.7 | 363.3±141.4 | 440.6±116.4 | 0.002 |
| Implant placement | 0.314 | |||
| Subpectoral | 106 (87.6) | 56 (84.9) | 50 (90.9) | |
| Prepectoral | 15 (12.4) | 10 (15.1) | 5 (9.1) | |
| Implant shape | 0.221 | |||
| Anatomical | 118 (96.7) | 66 (98.5) | 52 (94.6) | |
| Expander | 4 (3.3) | 1 (1.5) | 3 (5.4) | |
| Surgical procedure** | ||||
| Skin-sparing mastectomy | 75 (61.5) | 52 (77.6) | 33 (60.0) | <0.001 |
| Nipple-sparing mastectomy | 49 (40.2) | 16 (23.9) | 23 (41.8) | <0.001 |
| Radical mastectomy | 2 (2.0) | 2 (3.0) | 0 (0.0) | 0.501 |
| Sentinel lymph node biopsy | 7 (6.0) | 7 (10.4) | 0 (0.0) | 0.015 |
*, For one cancer patient, data on implant size and placement were not available in the medical chart. **, Note that a woman can contribute to multiple rows, given that one woman can have different operations on each breast.


Of the 67 therapeutic patients 18 (27%) had adjuvant chemotherapy, 12 (18%) had anti-hormone therapy and 2 (3%) had radiation therapy. Thirty-five (52%) therapeutic patients had no adjuvant therapy.
Number of corrective surgeries
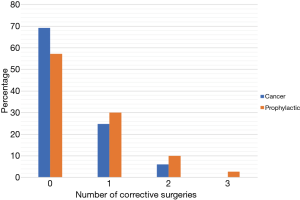
Of the 122 women 38% underwent additional surgery. During the mean follow up of 2.7 (range, 0.8–4.7) years the Poisson regression showed a 60% higher incidence rate (IRR =1.6) of having corrective surgery in the prophylactic group (P=0.016, 95% CI: 1.09–2.29) than in the therapeutic group.
Figure 3 illustrates the number of corrective surgeries in the two groups. Among the cancer patients 69% had no additional surgery, while 25%, 6% and 0% had one, two and three additional surgeries, respectively. The corresponding figures for the prophylactic treated women were 57%, 30%, 10% and 3% (P=0.073). The mean number of additional surgeries was 0.4 for the cancer group and 0.6 for the prophylactic treated women.
Types of corrective surgery
We calculated the frequency of each corrective surgery indication, as classified in the method section. In the therapeutic group the dominant indication for corrective surgery was asymmetry (53%), followed by thin skin flaps/visible implant (18%) and correction of the natural contralateral breast (10%). In the prophylactic treated women thin skin flaps/visible implant (49%) was the dominant indication, followed by asymmetry in size (23%) and wrong shape of implant (22%). The result is illustrated in Figure 4.
Discussion
In this cohort of 122 women undergoing mastectomy and direct to implant breast reconstruction by a single surgeon, we found that 69% of the therapeutic and 57% of the prophylactic treated women had no additional surgeries. Among the remaining, a higher incidence of corrective surgeries was found in the prophylactic treated women compared to the cancer patients.
The demographics in our study group differed in age, BMI and prevalence of hypertension. Both BMI and hypertension are correlated to age and the increased number of these in the cancer group can probably be explained by the age difference among the groups. This age difference was expected, given that the group of women with prophylactic risk reducing surgery often choose this at a young age. The cancer group consist of two subgroups: (I) a larger group of older women with sporadic occurrence of breast cancer. The average age will follow the age standardized rate ratios with peak incidence between 50–70 years of age (8). And (II) a smaller group of women with genetic risk of breast cancer, unrecognized until the occurrence of their first cancer. This smaller group will probably resemble the prophylactic treated women and tend to lower the mean BMI and hypertension among the cancer patients.
To the best of our knowledge only one other study has presented number of corrective surgeries following single stage breast reconstruction and stratified into prophylactic and therapeutic mastectomy (9). Nurudeen et al. included 28 women reconstructed with single stage implant breast reconstruction. They found that 9/28 (32%) women undergoing risk reduction mastectomy had no additional surgery, while four, seven and five women had one, two and three additional surgeries, respectively. For women undergoing therapeutic mastectomies 8/10 (80%) had no additional surgeries while two women had one additional revision surgery. Although these data are very limited, it is in line with our results.
Several studies have reviewed either implant-based reconstruction or autologous breast reconstruction. Eom et al., reviewed 185 women reconstructed during 2005–2009 and found a mean number of secondary operations per breast of 2.37 to complete breast reconstruction (10). Considerably higher than in our study. They included multiple reconstruction methods and nipple reconstruction, which was not included in our study. Only a few were at that time reconstructed with a mesh, making comparison even more difficult. Enajat et al. studied additional surgeries in women reconstructed with DIEP and SIEA flaps (11). They found an overall number of additional surgeries for aesthetical refinement of 2.17 per women. Kim et al. investigated the number of corrective surgeries following abdominal free flap breast reconstruction and found that 39% had additional surgery. The average number of surgeries was 0.5 and thus more similar to our findings (12).
Our study sample consisted of 67 patients with breast cancer and 55 patients with genetic disposition for breast cancer. Both groups received the same surgical treatment, by the same surgeon and the same follow-up with the same offer of corrective surgery. The time leading up to the treatment was very different for the two groups. The psychological concerns and physical distress following a cancer diagnosis and treatment is only prominent in one of our study groups. Many of the cancer patients are additionally facing chemotherapy, axillary lymph node staging and anti-hormone treatment. One could hypothesize that all these procedures prior to mastectomy and breast reconstruction might influence the choice to have more elective surgery following treatment. It is also possible that the patients in the cancer group are more easily satisfied with the result and have lower expectations concerning aesthetic outcome. Studies support this hypothesis by defining a response shift in women with a breast cancer diagnosis. After a diagnosis of breast cancer, women frequently report a change in their priorities, how they look at life, and what they value. As a result, factors that used to cause dissatisfaction may no longer do so (13,14). This response shift could contribute to higher levels of satisfaction reported in women with breast cancer compared to women treated prophylactically. Other studies have also shown that women with breast cancer have no explicit expectations regarding surgery because their focus at that time was on surviving cancer rather than on reconstruction (3). The patients in the prophylactic group have never experienced breast cancer or the treatment associated with it. Not having the same psychological burden as a patient with breast cancer, might lead to more concerns about the aesthetic outcome and more willingness to undergo corrective surgery.
Patients choosing corrective surgery, do so because the aesthetic outcome of the reconstruction does not match their expectations or needs. Studies have shown that appearance is a key factor for women when deciding if reconstruction was better or worse than expected (13,15-17). Some appearance-related concerns or dissatisfaction with the aesthetic outcome can be mended with corrective surgery, but some of these concerns could possibly have been prevented with better information and expectation management prior to surgery. Studies have shown that appearance-related concerns reported by women suggest that they did not fully understand how different their reconstructed breast might look or feel, particularly after implant-based reconstruction (15). This study further implicates the need for thorough patient information and managing expectations before surgery, especially in those patients receiving prophylactic mastectomy and reconstruction, since they receive a higher number of corrective surgeries. Detailed education of this group, where fast decision is not needed, will allow patients to better shape their expectations. Patients need to be advised of the frequent need for additional surgery. Around every second women will need additional surgery and multiple surgeries are not unusual.
More studies are needed to explore the predictors and outcome measurements for receiving corrective surgery following breast reconstruction. It would also be interesting to investigate the patient satisfaction following corrective surgery. A limitation to our study is the relatively short follow up, which could impact the results. More studies could investigate whether the number of corrective surgeries will equalize over time.
Multiple surgeries following direct to implant breast reconstruction is frequent. Woman receiving prophylactic mastectomy were more likely to have corrective surgery compared to women receiving therapeutic mastectomy. This is important information in the consultation process prior to the reconstructive surgery.
Conclusions
Direct to implant breast reconstruction are frequently followed by one or multiple additional corrective surgeries among breast cancer patients and certainly among women treated with risk reducing mastectomy. It is of great importance to discuss this with the patient prior to surgery in order to create realistically balanced expectations. The range of aesthetic outcomes, risk of complications, the potential need for corrective surgery and the different types of possible corrective surgery should be included.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/abs-20-63
Data Sharing Statement: Available at http://dx.doi.org/10.21037/abs-20-63
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/abs-20-63). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the Danish Patient Safety Authority (3-3013-2117/1) and The Danish Data Protection Agency (17/15192). The study was conducted in accordance with the declaration of Helsinki (as revised in 2013) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- DeSantis CE, Ma J, Goding Sauer A, et al. Breast cancer statistics, 2017, racial disparity in mortality by state. CA Cancer J Clin 2017;67:439-48. [Crossref] [PubMed]
- Casella D, Di Taranto G, Marcasciano M, et al. Evaluation of prepectoral implant placement and complete coverage with TiLoop bra mesh for breast reconstruction: a prospective study on long-term and patient-reported BREAST-Q outcomes. Plast Reconstr Surg 2019;143:1e-9e. [Crossref] [PubMed]
- Nissen MJ, Swenson KK, Kind EA. Quality of life after postmastectomy breast reconstruction. Oncol Nurs Forum 2002;29:547-53. [Crossref] [PubMed]
- Frost MH, Hoskin TL, Hartmann LC, et al. Contralateral prophylactic mastectomy: long-term consistency of satisfaction and adverse effects and the significance of informed decision-making, quality of life, and personality traits. Ann Surg Oncol 2011;18:3110-6. [Crossref] [PubMed]
- Razdan SN, Patel V, Jewell S, et al. Quality of life among patients after bilateral prophylactic mastectomy: a systematic review of patient-reported outcomes. Qual Life Res 2016;25:1409-21. [Crossref] [PubMed]
- Zabora J. The prevalence of psychological distress by cancer site. Psychooncology 2001;10:19-28. [Crossref] [PubMed]
- Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377-81. [Crossref] [PubMed]
- Association of the Nordic Cancer Registries; Danish Cancer Society. NORDCAN: Cancer Incidence, Mortality, Prevalence and Survival in the Nordic Countries, Version 8.1 (28.06.2018). Available online: http://www.ancr.nu
- Nurudeen S, Guo H, Chun Y, et al. Patient experience with breast reconstruction process following bilateral mastectomy in BRCA mutation carriers. Am J Surg 2017;214:687-94. [Crossref] [PubMed]
- Eom JS, Kobayashi MR, Paydar K, et al. The number of operations required for completing breast reconstruction. Plast Reconstr Surg Glob Open 2014;2:e242 [Crossref] [PubMed]
- Enajat M, Smit JM, Rozen WM, et al. Aesthetic refinements and reoperative procedures following 370 consecutive DIEP and SIEA flap breast reconstructions: important considerations for patient consent. Aesthetic Plast Surg 2010;34:306-12. [Crossref] [PubMed]
- Kim EK, Suh YC, Maldonado AA, et al. Patients' aesthetic concerns after horizontally placed abdominal free flap breast reconstruction. Aesthetic Plast Surg 2015;39:686-93. [Crossref] [PubMed]
- Frost MH, Slezak JM, Tran NV, et al. Satisfaction after contralateral prophylactic mastectomy: the significance of mastectomy type, reconstructive complications, and body appearance. J Clin Oncol 2005;23:7849-56. [Crossref] [PubMed]
- Sprangers MA, Schwartz CE. Integrating response shift into health-related quality of life research: a theoretical model. Soc Sci Med 1999;48:1507-15. [Crossref] [PubMed]
- Steffen LE, Johnson A, Levine BJ, et al. Met and unmet expectations for breast reconstruction in early posttreatment breast cancer survivors. Plast Surg Nurs 2017;37:146-53. [Crossref] [PubMed]
- Andrade WN, Baxter N, Semple JL. Clinical determinants of patient satisfaction with breast reconstruction. Plast Reconstr Surg 2001;107:46-54. [Crossref] [PubMed]
- Elder EE, Brandberg Y, Björklund T, et al. Quality of life and patient satisfaction in breast cancer patients after immediate breast reconstruction: a prospective study. Breast 2005;14:201-8. [Crossref] [PubMed]
Cite this article as: Dissing J, Schierbeck J, Möller S, Bille C. Corrective surgeries following prophylactic and therapeutic mastectomy with immediate breast reconstruction. Ann Breast Surg 2020;4:21.

