Delayed free deep inferior epigastric perforator flap reconstruction following a bilateral nipple-sparing mastectomy: a case report
Introduction
The lifetime risk of developing breast cancer for a woman is approximately 12%, and the treatment of this pathway often includes mastectomy, which can lead to feelings of mutilation, decreased self-esteem, and loss of femininity (1-3). Thus, an important part of breast cancer therapy is reconstruction (4), which can be accomplished with either synthetic or autologous implants. Deep inferior epigastric perforator (DIEP) flaps have become the gold standard in autologous breast reconstruction (3,5-7). DIEP flaps are created from harvested abdominal subcutaneous tissues along with the associated perforating inferior epigastric vessels, while sparing the rectus abdominis muscle, and then translocated into the breast to replace the tissues removed during mastectomy and restore breast symmetry (7). While originally created for reconstruction after a total mastectomy, advances in technique and technology have made it possible for these flaps to also be used in both skin-sparing and nipple-sparing mastectomy, typically immediately post-mastectomy (primary), and less commonly, in the months following the procedure (secondary) (5,7-9). Here, we present a 52-year-old female with a history of bilateral nipple-sparing mastectomy who received a delayed breast reconstruction with free DIEP flaps one year post-procedure. Her case is unique because of the reconstruction timeline—her DIEP reconstruction took place sixteen months after a bilateral nipple-sparing mastectomy, which allowed adequate time for further therapy and recovery. Most DIEP reconstructions after nipple-sparing mastectomy occur immediately or soon after the initial procedure; however, there is no standardization on the timing of reconstruction in the setting of adjuvant therapy (10). We present the following article in accordance with the CARE reporting checklist (11) (available at http://dx.doi.org/10.21037/abs-20-60).
Case presentation
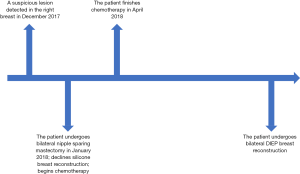
A 51-year-old G3P2 female presented in December 2017, with 2.1 cm right upper outer quadrant mass and a 1.3cm right axillary lymph node on screening mammogram, with no suspicious lesions in the left breast. The presence of the mass was confirmed with ultrasound, and biopsy revealed a grade 3 invasive mammary carcinoma and a benign lymph node. In January 2018, the patient underwent bilateral nipple-sparing mastectomy (via inframammary incisions) with right axillary sentinel lymph node biopsy, which was completed without complication, and bilateral tissue expanders were immediately placed. Post-operative pathologic staging was stage IIa, T2N0M0G3, ER 1%, PR 0%, HER2/neu negative invasive adenocarcinoma of the right breast. The patient was initially offered silicone implant breast reconstruction, which she declined. Thus, the patient began the first of four cycles, each dosed at 1 mg × 150 taxotere and 100 mg × 12 cyclophosphamide (TC) chemotherapy in January of 2018 and finished in April 2018.
After completing chemotherapy, the patient elected to undergo autologous breast reconstruction. Bilateral DIEP breast reconstruction was completed without complication in May 2019. To date, the patient continues to show no signs of breast cancer recurrence and expresses satisfaction in the aesthetic outcome of the procedures (see Figures 1-3). The patient experienced no adverse or unanticipated events during the course of her treatment (see Figure 4).
She has consented to images and other clinical information related to her case to be reported in a medical publication. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Discussion
Decisions regarding post-mastectomy breast reconstruction are both medically and emotionally complicated. Decisions regarding timing and type of reconstruction are directed by patient preference and influenced by factors such as adjuvant therapy plans, capabilities of the reconstruction team, and the patient’s body characteristics and overall health (12). Delayed bilateral free DIEP flap reconstruction of the breast after nipple-sparing mastectomy provides an option for eligible patients to maintain their native nipple and areolar complex, which has been shown to result in significantly improved patient satisfaction scores (13,14), while still receiving an autologous breast reconstruction. This delayed approach to reconstruction could be ideal in patients who desire autologous reconstruction but require postmastectomy radiotherapy, as improved results have been demonstrated in patients who undergo delayed reconstruction in that described setting (15-18). This technique may also prove useful in any other setting that prohibits a patient from receiving immediate postmastectomy breast reconstruction.
From this patient’s experience, we conclude that secondary DIEP flap reconstruction after nipple-sparing mastectomies is an acceptable treatment pathway in breast cancer patients and may be preferable for outcomes in cases that require postmastectomy radiation therapy.
Limitations
The strength of this case report is the documentation of an uncomplicated case with good outcomes that describes a technique of secondary DIEP flap reconstruction in a bilateral nipple-sparing mastectomy. The limitations of the study are similar to limitations of all case studies; it is limited to a single patient and is therefore not generalizable to the entire population. However, it does provide an example of a non-habitual reconstructive technique for further studies.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/abs-20-60
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/abs-20-60). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Disclaimer: The opinions and assertions contained herein are those of the authors and do not reflect those of the Uniformed Services University, the United States Army, or the Department of Defense.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gilboa D, Borenstein A, Floro S, et al. Emotional and psychosocial adjustment of women to breast reconstruction and detection of subgroups at risk for psychological morbidity. Ann Plast Surg 1990;25:397-401. [Crossref] [PubMed]
- Macadam SA, Zhong T, Weichman K, et al. Quality of Life and Patient-Reported Outcomes in Breast Cancer Survivors: A Multicenter Comparison of Four Abdominally Based Autologous Reconstruction Methods. Plast Reconstr Surg 2016;137:758-71. [Crossref] [PubMed]
- Leyngold MM. Is Unipedicled Transverse Rectus Abdominis Myocutaneous Flap Obsolete Owing to Superiority of DIEP Flap? Ann Plast Surg 2018;80:S418-S420. [Crossref] [PubMed]
- Hauck T, Horch RE, Schmitz M, Arkudas A. Secondary breast reconstruction after mastectomy using the DIEP flap. Surg Oncol 2018;27:513. [Crossref] [PubMed]
- Fujimoto H, Ishikawa T, Satake T, et al. Donor site selection and clinical outcomes of nipple-areola skin-sparing mastectomy with immediate autologous free flap reconstruction: A single-institution experience. Eur J Surg Oncol 2016;42:369-75. [Crossref] [PubMed]
- Laporta R, Longo B, Sorotos M, et al. Time-dependent factors in DIEP flap breast reconstruction. Microsurgery 2017;37:793-9. [Crossref] [PubMed]
- Yano K, Hosokawa K, Nakai K, et al. Skin-sparing mastectomy and immediate reconstruction with a deep inferior epigastric perforator flap. Breast Cancer 2003;10:275-80. [Crossref] [PubMed]
- Cho HJ, Kwon HJ, Moon SH, et al. One-stage nipple and breast reconstruction using a deep inferior epigastric perforator flap after a skin-sparing mastectomy. Arch Plast Surg 2020;47:26-32. [Crossref] [PubMed]
- Satake T, Sugawara J, Yasumura K, et al. "Mini-Flow-Through" Deep Inferior Epigastric Perforator Flap for Breast Reconstruction with Preservation of Both Internal Mammary and Deep Inferior Epigastric Vessels. Arch Plast Surg 2015;42:783-7. [Crossref] [PubMed]
- Weber WP, Haug M, Kurzeder C, et al. Oncoplastic Breast Consortium consensus conference on nipple-sparing mastectomy. Breast Cancer Res Treat 2018;172:523-37. [Crossref] [PubMed]
- Riley DS, Barber MS, Kienle GS, et al. CARE guidelines for case reports: explanation and elaboration document. J Clin Epidemiol 2017;89:218-35. [Crossref] [PubMed]
- Djohan R, Gage E, Bernard S. Breast reconstruction options following mastectomy. Cleve Clin J Med 2008;75:S17-S23. [Crossref] [PubMed]
- Yoon-Flannery K, DeStefano LM, De La Cruz LM, et al. Quality of life and sexual well-being after nipple sparing mastectomy: A matched comparison of patients using the breast Q. J Surg Oncol 2018;118:238-42. [Crossref] [PubMed]
- Bailey CR, Ogbuagu O, Baltodano PA, et al. Quality-of-Life Outcomes Improve with Nipple-Sparing Mastectomy and Breast Reconstruction. Plast Reconstr Surg 2017;140:219-26. [Crossref] [PubMed]
- Fertsch S, Munder B, Hagouan M, et al. Immediate-DElayed AutoLogous (IDEAL) Breast Reconstruction with the DIEP Flap. Chirurgia (Bucur) 2017;112:387-93. [Crossref] [PubMed]
- O'Connell RL, Di Micco R, Khabra K, et al. Comparison of Immediate versus Delayed DIEP Flap Reconstruction in Women Who Require Postmastectomy Radiotherapy. Plast Reconstr Surg 2018;142:594-605. [Crossref] [PubMed]
- Skraastad BK, Knudsen C, Jackson C, et al. Quality of life, patient satisfaction and cosmetic outcome after delayed breast reconstruction using DIEP flap: a 10 years' follow-up survey. J Plast Surg Hand Surg 2019;53:119-24. [Crossref] [PubMed]
- Sosin M, Gulla A, Potdevin L, et al. Timing of radiation therapy in nipple-sparing mastectomy influences outcomes and patient-reported quality of life. Breast J 2018;24:934-9. [Crossref] [PubMed]
Cite this article as: Hansen J, Lin-Hurtubise K. Delayed free deep inferior epigastric perforator flap reconstruction following a bilateral nipple-sparing mastectomy: a case report. Ann Breast Surg 2020;4:20.