
Reduction of postoperative opioid use in oncologic breast surgery and the creation of multimodal pain management guidelines and practices
Introduction
The history of opioid-based pain management and breast surgery
Opioid use for pain management in the medical world began in ancient Sumeria around the year 3400 BC with the cultivation of the poppy plant. Throughout the 19th century, opioid analgesics, such as morphine, were both easily accessible and commonly misused. For the majority of the 20th century, opioid abuse and its utilization for medicine were transformed with numerous regulatory constraints, limiting addiction and overdose. However, since 1990, the prescription of opioids for medical use and the illicit trade of opioids has skyrocketed, culminating in the current opioid public health emergency. The relatively recent surge in prescription opioid diversion and misuse is fueled, partially, by changes in prescribing practices of opioid medications and the adoption of more potent modern opioids, such as fentanyl and oxycodone (5).
During this timeframe, breast oncological theory and surgery have seen advancement. The evolution of oncologic breast surgery can be followed from the first Halsted radical mastectomy, performed in 1882, to the less disfiguring modified radical mastectomy introduced in 1932. Ultimately, this evolution has culminated with the 1985 discovery that women with early-stage breast cancer treated with lumpectomy and radiation have similar survival rates (6). In addition, advancement in the oncological treatment of the axilla is evidenced in the transition from radical axillary dissections to the sentinel lymph node (SLN) biopsy procedure adopted as recently as the 1990s (7). In summary, breast cancer surgery is becoming less invasive with the implementation of novel surgical techniques, technologies, and theory.
Despite advancements in the potency of opioid analgesics and in numerous breast surgery techniques, societal interactions with opioids has been quite disastrous, as corroborated by the current state of public health emergency (1,2). The crisis seems to be supported, in part, by the opioid prescribing habits of physicians across the country (2-4). Even though there have been nascent efforts by federal and state governments to assist in regulating these opioid prescribing practices, there is little current evidence of the efficacy of these regulations in adequately addressing opioid over-prescription and providing feasible analgesic alternatives to opioids for acute surgical pain (8). Currently, the Department of Health and Human Services and the CDC lists chiropractic, acupuncture, and meditation as some alternatives to opioid analgesics for both acute and chronic pain (8).
Thus, it appears that the responsibility of curbing the flow of opioids into the general US populace and optimizing pain management for their patients is in the hands of the prescribing physician.
Analgesic alternatives for postoperative acute surgical pain management
Liposomal bupivacaine analgesics have been used in a wide range of surgical procedures, leading to a reduction of postoperative opioid usage and an improvement in pain control (9). These benefits translate to improved patient satisfaction, less opioid-related side effects/complications, and lower patient pain indexes (10). However, there have been no targeted studies proving the benefit of liposomal bupivacaine specifically for oncologic breast surgery. Furthermore, there has been no mention of the use of liposomal bupivacaine in smaller breast cases, such as partial mastectomy, partial mastectomy with SLN biopsy, open excisional surgical breast biopsy, or mastectomy without reconstruction. Often these patients with historically “less painful” procedures experience more pain due to incomplete perioperative pain management (11,12). In our study, we explored the possibility of incorporating liposomal bupivacaine admixed with bupivacaine HCl as the primary perioperative analgesic for three of the most prevalent breast oncological surgery types to aid in postoperative pain management.
Liposomal bupivacaine operates by extending “the duration of local anesthetic action by slow release from the liposome and delays the peak plasma concentration when compared to plain bupivacaine administration”. On average the analgesic effect lasts 96 hours (4 days). Depending on the site and dosage administered, the analgesic benefit may last for up to 5 days or more (13,14). Various studies have exhibited liposomal bupivacaine to be an extremely effective postoperative pain relief tool with “opioid sparing effects” and “an acceptable adverse effect profile” (9,10).
To date, there have been few if no medically-proven guidelines set to appropriately describe the amount of opioid analgesic needed for the pain management for specific surgery types. The objective of this study is to establish opioid prescribing guidelines in an attempt to create an appropriate mandate for postoperative opioid-based pain management for oncologic breast patients. This can be attained by incorporating liposomal bupivacaine as an operatively delivered postoperative analgesic. We intend to prove that not only can the postoperative use of opioids be decreased with the aid of liposomal bupivacaine, their entire elimination is possible in a high percentage of patients undergoing certain breast oncological surgeries. Selective studies addressing specific surgery types are needed to appropriately set opioid prescribing guidelines and practices.
Methods
Over a 24 month period, July 1, 2017 to June 30, 2019, postoperative opioid usage and self-reported postoperative pain data was collected retrospectively from 264 female oncologic breast surgery patients in Hillsborough County, Florida. All of the patients were operated on by the same breast surgeon at one of three medical facilities in Hillsborough County, Florida. The entire patient population consisted of females ranging in age from 18 to 91 years old.
The IRB was consulted at the onset of the study, who determined that the data was an internal review of office practice patterns and IRB approval was not necessary.
Division of patients into three surgery types
Patients were divided into three categories. These are composed of patients with breast-conserving surgery namely partial mastectomy with SLN including and not including axillary dissection. The patients’ tumors were localized by palpation or radiologic guidance using either wire localization or a surgical guidance system (SGS), specifically the SAVI ScoutTM. In the majority of these patients an axillary dissection was not necessary. A few patients in this category had a partial mastectomy alone without a concomitant SLN biopsy.
The second category consists of patients who underwent mastectomy. The tracked patient data included the laterality of their procedure, if a SLN biopsy including or not including axillary dissection occurred during the mastectomy, and whether they received immediate breast reconstruction.
The third category included patients that had an excisional surgical biopsy with or without wire or SGS localization.
Non-oncologic breast surgical operations, for example MediportTM and needle core biopsy procedures, were excluded from the study. The entirety of the patients for each type of surgery was cared for by the same oncologic breast surgeon.
Postoperatively, all patients were prescribed either the opioid oxycodone/acetaminophen 5/325 mg, hydrocodone/acetaminophen 5/325 mg, or tramadol 50 mg based on allergy and/or patient choice. From July 1, 2017 until December 31, 2017 each patient was prescribed 20 opioid pills and from January 1, 2018 until June 30, 2019 each patient was prescribed 12 opioid pills.
Patients were directly instructed by the prescribing physician to resort to over-the-counter analgesics, choosing between ibuprofen, naproxen, or acetaminophen, before using their prescribed opioid for breakthrough pain. If no postoperative pain was experienced, patients were instructed not to take any analgesics.
Liposomal bupivacaine administered operatively
The totality of the patients in the study received the liposomal bupivacaine as an operatively administered analgesic unless otherwise specified. Liposomal bupivacaine is the first long acting non-opioid local anesthetic approved by the FDA, October 2011 (14).
The general technique for a field block injection of liposomal bupivacaine is a “moving needle” technique using a 25-gauge needle or larger to prevent liposomal disruption upon infusion (10). Liposomal bupivacaine does not diffuse into the tissue as easily as bupivacaine HCl due to the viscous nature of the liposomes. Thus, the analgesic is deposited into the tissue in the relative location where the injection occurs. Therefore, in order to assure adequate coverage of all exposed surfaces the needle needs to move along all exposed surfaces slowly while the agent is injected.
In our study the conditions under which patients did not receive liposomal bupivacaine include patient allergy, or lack of liposomal bupivacaine on formulary. In addition, patients who received liposomal bupivacaine from a different provider during a combined case were excluded from the study. Open surgical biopsy patients not receiving liposomal bupivacaine did receive an alternative local anesthetic consisting of 0.25% bupivacaine HCl mixed 1:1 with 1% lidocaine. A field block was performed injecting a total of 30cc evenly into the skin and all exposed surfaces.
Liposomal bupivacaine surgical injection technique
For the patients who received liposomal bupivacaine the same injection technique was used for all patients by the same surgeon.
A single-dose administration using a 266 mg (20 mL) vial of liposomal bupivacaine admixed with 0.25% or 0.5% bupivacaine HCl was utilized. The bupivacaine HCl expanded the volume of the injectable solution to ensure sufficient coverage of larger surfaces and to enhance the immediate analgesic effect. The volume of bupivacaine HCl added to our liposomal bupivacaine ranged from 10 cc for an open excisional surgical biopsy, 30 cc for a partial mastectomy with SLN or unilateral mastectomy, and 60 cc for a bilateral mastectomy.
The liposomal bupivacaine mixture was injected via a 22 gauge needle using the “moving needle” field block technique to adequately insure even coverage of skin and all exposed surfaces.
For the open surgical biopsy and partial mastectomy with SLN approximately 5cc of liposomal bupivacaine was injected at the anticipated incision site prior to all new incisions, and the remainder was injected equally into all exposed surfaces before closure. During a SLN biopsy or axillary dissection, if the pectoralis major and/or serratus anterior muscle or if the first intercostal brachial sensory nerve were exposed, these sites were injected as well.
For a mastectomy, the “moving needle” technique injections covered the entire surgical field including the axilla, serratus anterior muscle, the pectoralis major muscle, and the superior and inferior skin flaps. For a bilateral mastectomy, the liposomal bupivacaine mixture was divided equally and injected evenly on both sides. The skin was not injected prior to incision; all surfaces including skin were injected before closure.
Data collection and analysis through the use of interpersonal survey and Mathematica™
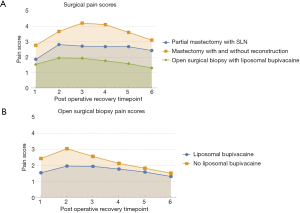
Patients were given a pain survey to complete at their postoperative examination. Oncologic patients, including patients who had a mastectomy or partial mastectomy with SLN, were examined on postoperative day 7 while open excisional surgical biopsy patients were examined on postoperative day 14. The information gathered by the survey included if, which, and how much postoperative pain medication the surveyed patient took, distinguishing between opioid (namely hydrocodone, oxycodone, or tramadol) and non-opioid (namely ketorolac tromethamine, ibuprofen, naproxen, and acetaminophen) analgesics. The amount of analgesic taken was recorded and tabulated in the unit of “pills consumed” and, for opioid medications oxycodone and tramadol, converted to proportional quantity of hydrocodone. Patients were also asked to quantify their level of pain at different time intervals after surgery using the externally validated 11-point Numerical Pain Rating Scale (NPRS) of 0–10 with 0 denoting no pain and 10 denoting worst imaginable pain (15,16). Their pain indexes/scores were recorded at these timepoints (Figure 1): recovery room, night of surgery, postoperative day 1, 3, 5, and 7. The survey was completed by the patients at their postoperative appointment and reviewed during an interpersonal interview with the breast surgeon.
The resulting data collected through the survey and interview was tabulated and analyzed using the data processing program Mathematica™.
Results
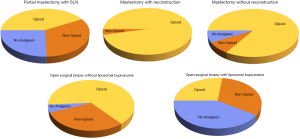
There were a total of 264 patients involved in the study who received either a partial mastectomy with SLN, mastectomy (with or without reconstruction), or an open surgical biopsy (with or without liposomal bupivacaine). Of the total, 46.6% of the oncologic breast patients opted to take some form of opioid in their personal pain management regimen, with 26.1% and 27.3% opting to take no analgesic and non-opioid analgesics respectively. When comparing the three surgery types, the liposomal bupivacaine eliminated postoperative analgesic use most effectively for the open surgical biopsy, somewhat in partial mastectomy with SLN and rarely for the total mastectomy.
Partial mastectomy with SLN biopsy
For this portion of the study, a total of 86 patients were surveyed about their analgesic use over a 7-day period starting immediately after their surgery. All of the 86 patients were injected with the liposomal bupivacaine described in the methods section of this study. Approximately 42% of the partial mastectomy with SLN patients elected to take either hydrocodone, oxycodone, or tramadol with or without some sort of supplemental non-opioid medication. The remaining 62% of patients took only non-opioid or no analgesic (33% and 26% respectively) during their surgical recovery (Figure 2). For both of the subsets of patients who opted to take opioid analgesics and only non-opioids during their postoperative pain management regimen, both groups took approximately 2 pills per day over a total of 3 days.
Open surgical biopsy
For this portion of the study, there exists two corresponding groups of patients. The first population is comprised of 20 patients who received no liposomal bupivacaine during their surgery. In this group, 65% of patients took opioid while 30% of patients used only non-opioid analgesics. In total, only 5% used no analgesic during their recovery from surgery (Figure 2).
The group of patients who received liposomal bupivacaine during their open surgical biopsy is comprised of 108 patients. Only 27% of patients in this group used opioid analgesics, while 32% and 41% took only non-opioid or no analgesic respectively (Figure 2).
Of the group of patients who received liposomal bupivacaine, approximately one in every four patients opted to take opioid analgesics. Comparatively, slightly more than half of the patients in the population who did not receive liposomal bupivacaine opted to take opioid analgesics in their personal pain management regimen. Thus, the group that received liposomal bupivacaine during their surgery had a 50% reduction in the portion of patients who opted to take opioid analgesics. Additionally, the patients in both groups who took opioids (the patients who both received and did not receive liposomal bupivacaine) had the same approximate regimen of 2 pills per day over a total of 3 days.
Total mastectomy with and without reconstruction
For this portion of the study, the surgery type was divided into two equal groups of 25 patients along the criterion of if the mastectomy was paired with an immediate surgical reconstruction of the breast(s) or not. The group of patients that underwent reconstruction were almost entirely bilateral mastectomy cases, while the group of patients who did not undergo reconstruction contain an approximately even proportion of unilateral and bilateral mastectomy cases.
For the group of patients who received reconstruction, 96% (24 out of 25 patients) took some form of opioid analgesic, while 4% took non-opioid analgesics (Figure 2). For the group of patients who did not receive reconstruction, the percentage of the population that took some form of opioid analgesic was a majority, with 84% (21 out of 25 patients) electing to take opioids during their recovery. Of the remaining four patients in this group, two opted to take non-opioid analgesics while the other two took no analgesic, composing of 16% of the total population (Figure 2).
The total mastectomy group who did receive reconstruction took an approximate average of 4 opioid pills over a total of 6 days, while those who did not receive reconstruction took an approximate average of 2.5 opioid pills over a total of 3 days.
Postoperative pain indexes
While lowering the patients’ perceived pain index during their postoperative recovery was not the primary purpose of the study, the patients of most every surgery type never experienced an average pain score higher than 4, largely regarded as sufficient for return to normal activities (17,18). Specifically, it appears that the liposomal bupivacaine was effective at delaying the peak postoperative acute pain experienced by the patients while also diminishing the average pain index at every postoperative recovery time interval, as clearly portrayed in Figure 1B. The efficacy of liposomal bupivacaine for the partial mastectomy with SLN and total mastectomy is expressed by a reduction of postoperative patient pain. Prior studies indicate that the pain indexes normally experienced on postoperative day 1 for the partial mastectomy with SLN range from 2–5 (mean of 3) as well as 1.5–6 (mean of 4) and 1–5 (mean of 3) for a total mastectomy with and without reconstruction respectively. The pain indexes recorded in our study are markedly less than that which is usually associated with these common breast oncologic surgeries (18,19).
Discussion
In the modern, opioid-based pain management scheme, physicians are thrust in an immensely overwhelming situation of balancing responsibility for postoperative pain management of their patients while conforming to the constraints of the new controlled substance legislation resulting from the current opioid crisis. As of 2018, eight US states have issued emergency declarations pertaining to the opioid crisis, with many introducing new strict prescribing guidelines for physicians. Florida, for example, limits acute pain opioid prescriptions to no more than 3 days with a 7-day exemption for patients with justifiable cause (20). Currently, there are few scientific studies that attempt to provide medically-proven guidelines for pain management designed to assist the prescribing surgeons to conform to the opioid crisis era legislative guidelines while still providing constructive means of pain management to their patients (20,21). Cognizant of this void, this study aims to set applicable and medically-proven postoperative pain treatment guidelines for oncologic breast surgery patients while testing possible auxiliary means of pain management to create a multimodal analgesic regimen to reduce opioid use.
All of the prescribing guidelines below are based on a unit pill scale of hydrocodone/acetaminophen 5/325 mg. Additionally, every guideline is designed to cover 100% of the group of patients who received that specified surgery excluding outlying patients denoted in Figure 3. Listed along with the prescribing guidelines are the percentage of patients who opted to take opioid analgesics for each surgery type. Based on the data in Figure 3 and Table 1, our recommended opioid prescribing guidelines are below, followed by our recommended application of said guidelines:
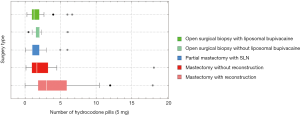
Table 1
| Range | Partial mastectomy with SLN | Open surgical biopsy with liposomal bupivacaine | Open surgical biopsy without liposomal bupivacaine | Mastectomy with reconstruction | Mastectomy without reconstruction |
|---|---|---|---|---|---|
| Minimum | 0.3 | 0.5 | 0.11 | 0.15 | 0 |
| 25% | 1.0 | 1.56 | 1.0 | 1.0 | 1.88 |
| Medium | 1.25 | 2.0 | 1.0 | 1.67 | 3.0 |
| 75% | 2.0 | 2.08 | 2.0 | 3.25 | 5.86 |
| Maximum | 6.67 | 6.06 | 6.0 | 18.18 | 18.01 |
- Open surgical biopsy without liposomal bupivacaine: 3 pills (65%);
- Open surgical biopsy with liposomal bupivacaine: 3 pills (27%);
- Partial mastectomy with SLN with liposomal bupivacaine: 4 pills (42%);
- Mastectomy without reconstruction with liposomal bupivacaine: 5 pills (84%);
- Mastectomy with reconstruction with liposomal bupivacaine: 11 pills (96%).
These guidelines were formulated with the intent of sufficiently supporting the opioid-based personal pain management regimen of all the patients of each specified surgery type, excluding outliers. Therefore, the guidelines are best suited for the most invasive breast oncologic surgeries, such as mastectomy with/without reconstruction, because the majority of the patients (80% or more on average) opt to take their opioid prescription. But, for the least invasive surgeries, such as the open surgical biopsy with liposomal bupivacaine and the partial mastectomy with SLN, these guidelines represent how to best fulfill the opioid need of a relative minority of patients (approximately 40% or less on average). So, when applying the guidelines for the least invasive oncologic breast surgeries, the prescribing physician could educate the patient that non-opioid analgesics are proven to be sufficient for the pain management of most of the patients who undergo this type of surgery and attempt to reduce the number of opioid prescriptions filled by allowing the patient to decide if they want to fill an opioid prescription. Additionally, opioid prescriptions for these kinds of surgeries could be handled on a need base system where the minority of patients who opt for opioid analgesics call their prescribing physician after their surgery.
Unless otherwise noted, these guidelines are designed to be utilized when paired with an operatively injected liposomal bupivacaine for the breast surgeries listed above. Even though the open surgical biopsy data in Table 1 appears to be equivalent with and without liposomal bupivacaine, these groups only represent the patients who took opioid analgesics. When patients received liposomal bupivacaine during an open surgical biopsy, they are about 2.5 times more likely (Table 2) to not take opioid analgesics during their personal pain management regimen. The data in Table 1 does not sufficiently portray this aspect of the liposomal bupivacaine in eliminating the use of postoperative opioid analgesics.
Table 2
| Categories | Partial mastectomy with SLN | Open surgical biopsy with liposomal bupivacaine | Open surgical biopsy without liposomal bupivacaine | Mastectomy with reconstruction | Mastectomy without reconstruction |
|---|---|---|---|---|---|
| Total patients | 86 | 108 | 20 | 25 | 25 |
| Percent opioid used | 36 (41.9%) | 29 (26.9%) | 13 (65.0%) | 24 (96.0%) | 21 (84.0%) |
| Pills per day | 1.75 | 1.79 | 2.15 | 3.85 | 2.36 |
| Average days | 3.25 | 2.66 | 2.85 | 5.75 | 3.29 |
| Compounding non-opioid days | 2.28 | 1.66 | 1.54 | 1.29 | 1.76 |
| Percent non-opioid used | 28 (32.6%) | 35 (32.4%) | 6 (30.0%) | 1 (4.0%) | 2 (8.0%) |
| Pills per day | 1.99 | 1.92 | 2.21 | 2.00 | 3.00 |
| Average days | 3.36 | 3.26 | 2.33 | 2.00 | 1.50 |
| No analgesic used | 22 (25.6%) | 44 (40.7%) | 1 (5.0%) | 0 (0%) | 2 (8.0%) |
According to the data in Tables 1 and 2, it appears that the liposomal bupivacaine was particularly apt at eliminating opioid use in the least invasive surgery types, such as the partial mastectomy with SLN and open surgical biopsy. However, the success of our proposed multimodal analgesic system and opioid guidelines cannot be solely quantified in the proportion of patients who took no analgesics but also should be expressed by the proportion of patients who were able to manage their acute pain with non-opioid analgesics. For the aforementioned less invasive surgery types, the proportion of patients who both took non-opioid and no analgesic are upwards of 30–35%. This constitutes a majority of patients (a 60–70% average) who did not utilize opioid analgesics postoperatively.
One of the best applications of liposomal bupivacaine for the reduction of prescription opioids is its utilization in relatively smaller, less invasive surgeries. It is in this realm that the largest reduction of opioid prescriptions per surgery type can be attained in common practice.
Besides skin cancer, breast cancer is the most commonly diagnosed cancer for American women with about 12% of the US female population developing invasive breast cancer in their lifetime. Of the 2019 predicted US population, roughly 20,000,000 women will develop invasive breast cancer, thus, leading them to undergo one of the oncologic breast surgeries covered in this study. So, having the ability to reduce the number and associated side effects of opioids as well as postoperative recovery time would be immensely, almost immeasurably impactful for the wellbeing of the US economy and population. This is our justification of the use of liposomal bupivacaine for relatively less invasive breast oncologic surgery (22,23).
Conversely, according to the data in Tables 1 and 2, it appears that liposomal bupivacaine is more beneficial at reducing postoperative opioid use in more invasive surgeries rather than eliminating it. Up until 2018, standard opioid prescribing habits in Hillsborough County, Florida allocated approximately 30–40 hydrocodone 5/325 mg pills for patients recovering from a total mastectomy. However, this is not to claim that liposomal bupivacaine does not reduce average opioid use for less invasive surgery as well. The median number of opioid pills taken after an open surgical biopsy without liposomal bupivacaine is almost double that with liposomal bupivacaine, but the range of pills for the patients who did take opioid analgesics is quite similar (ranging from 0 to 2 pills).
By curtailing the number of opioid pills needed for postoperative pain management with the use of liposomal bupivacaine, oncologic surgeons are better equipped to conform to the stringent opioid legislation being established both federally and statewide while limiting overprescribing habits, thus, helping to abate the circulation and diversion of opioids into society (20,24). The data exhibits that augmenting operative analgesic usage, such as with the application of liposomal bupivacaine, can have a beneficial effect on postoperative pain management, allowing opioid prescriptions to fall well below the newly mandated controlled substance guidelines.
Conclusions
It is time that we upgrade our operative and postoperative pain management strategies to reflect advancements in surgical techniques and patient treatment. As breast surgery becomes less invasive, relying on opioids to manage postoperative pain poses more risk to patients and society than reward. It is time that auxiliary modes of pain management, such as liposomal bupivacaine, and medically relevant guidelines inform oncologic opioid prescribing behavior.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/abs.2019.10.05). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The IRB was consulted at the onset of the study, who determined that the data was an internal review of office practice patterns and IRB approval was not necessary. Informed consent was waived due to the retrospective nature of the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Harlan E. Determination that a public health emergency exists. In: Services DoHaH, editor. Washington DC, 2017 Oct 26.
- Abuse NNIoD. Overdose death rates 2019 Jan. Available online: https://www.drugabuse.gov/related-topics/trends-statistics/overdose-death-rates
- Bohnert AS, Valenstein M, Bair MJ, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA 2011;305:1315-21. [Crossref] [PubMed]
- Hill MV, McMahon ML, Stucke RS, et al. Wide variation and excessive dosage of opioid prescriptions for common general surgical procedures. Ann Surg 2017;265:709-14. [Crossref] [PubMed]
- Rosenblum A, Marsch LA, Joseph H, et al. Opioids and the treatment of chronic pain: controversies, current status, and future directions. Exp Clin Psychopharmacol 2008;16:405-16. [Crossref] [PubMed]
- Cotlar AM, Dubose JJ, Rose DM. History of surgery for breast cancer: radical to the sublime. Curr Surg 2003;60:329-37. [Crossref] [PubMed]
- D'Angelo-Donovan DD, Dickson-Witmer D, Petrelli NJ. Sentinel lymph node biopsy in breast cancer: a history and current clinical recommendations. Surg Oncol 2012;21:196-200. [Crossref] [PubMed]
- Administration CfDCaPSAaMHS. Rx pain medications know the options-get the facts: managing your pain: which approach is right for you? Rockville MD 2017.
- Dasta J, Ramamoorthy S, Patou G, et al. Bupivacaine liposome injectable suspension compared with bupivacaine HCl for the reduction of opioid burden in the postsurgical setting. Curr Med Res Opin 2012;28:1609-15. [Crossref] [PubMed]
- Afonso AM, Newman MI, Seeley N, et al. Multimodal analgesia in breast surgical procedures: technical and pharmacological considerations for liposomal bupivacaine use. Plast Reconstr Surg Glob Open 2017;5:e1480 [Crossref] [PubMed]
- Joshi GP, Schug SA, Kehlet H. Procedure-specific pain management and outcome strategies. Best Pract Res Clin Anaesthesiol 2014;28:191-201. [Crossref] [PubMed]
- Joshi GP, Kehlet H. Procedure-specific pain management: the road to improve postsurgical pain management? Anesthesiology 2013;118:780-2. [Crossref] [PubMed]
- Pacira Pharmaceuticals. Exparel prescribing information. Parsippany NJ 2016.
- Pacira Pharmaceuticals. FDA advisory committee meeting briefing document [briefing document] 2018 Feb 14-15.
- Coté CJ, Lerman J, Anderson BJ. A practice of anesthesia for infants and children. Sixth edition. ed. Philadelphia, PA: Elsevier, 2019:1023-62.
- Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs 2005;14:798-804. [Crossref] [PubMed]
- Rosén HI, Bergh IH, Odén A, et al. Patients´ experiences of pain following day surgery - at 48 hours, seven days and three months. Open Nurs J 2011;5:52-9. [Crossref] [PubMed]
- Gerbershagen HJ, Aduckathil S, van Wijck AJ, et al. Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology 2013;118:934-44. [Crossref] [PubMed]
- Apfelbaum JL, Chen C, Mehta SS, et al. Postoperative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg 2003;97:534-40. [Crossref] [PubMed]
- Miller N. Florida's new opioid law: what you need to know. Orlando Sentinel 2018 Aug 14; Sect. Health.
- Rojas KE, Fortes TA, Flom PL, et al. Mastectomy is no longer an indication for postoperative opioid prescription at discharge. Am J Surg 2019;218:700-5. [Crossref] [PubMed]
- Limbach KE, Pommier SJ, Massimino KP, et al. A prospective study of opioid use for postoperative pain management after breast operation. Am J Surg 2020;219:8-14. [PubMed]
- Breastcancer.org. US breast cancer statistics Breastcancer.org 2019. Available online: http://www.breastcancer.org/symptoms/understand.bc/statistics
- Soelberg CD, Brown RE, Du Vivier D, et al. The US opioid crisis: current federal and state legal issues. Anesth Analg 2017;125:1675-81. [Crossref] [PubMed]
Cite this article as: Bridge DM, Bridge BA. Reduction of postoperative opioid use in oncologic breast surgery and the creation of multimodal pain management guidelines and practices. Ann Breast Surg 2019;3:27.

